Dapagliflozin and Sitagliptin Combination Therapy: An Overview of Clinical Utility in Type 2 Diabetes Mellitus with Multiple Cardiovascular Risk Factors
Article Information
L Ravikumar1, Ravindra S Kiwalkar2, Ravindra H S3, Beerakayala Lokesh4, Dhammdeep Dabhade5*
1Department of Cardiology, Parvati Seva Sadan, Cuttack, Odisha, India
2 R. Kiwalkar Medicare Centre Pune, Maharashtra, India
3Sreenidhi Diabetic Centre Bangalore, Karnataka, India
4Century Super Speciality Hospital, Hyderabad, Telangana, India
5Department of Medical Services, Emcure Pharmaceuticals Ltd. Maharashtra, India.
*Corresponding author: Dr. Dhammdeep C. Dabhade. Department of Medical Services, Emcure Pharmaceuticals Ltd. Pune, Maharashtra, India.
Received: 16 March 2023; Accepted: 23 March 2023; Published: 24 April 2023
Citation: L Ravikumar, Ravindra S Kiwalkar, Ravindra H S, Beerakayala Lokesh, Dhammdeep Dabhade. Dapagliflozin and Sitagliptin Combination Therapy: An Overview of Clinical Utility in Type 2 Diabetes Mellitus with Multiple Cardiovascular Risk Factors. Cardiology and Cardiovascular Medicine. 7 (2023): 141-144.
Share at FacebookAbstract
Cardiovascular disease remains the leading cause of mortality in patients with diabetes. Control of multiple cardiovascular risk factors in patients with type 2 diabetes mellitus often leads to substantial reduction in adverse cardiovascular events. Newer antihyperglycemic agents at several randomized controlled trials have demonstrated their cardiovascular safety along with reduction in cardiovascular outcomes in type 2 diabetes mellitus with or without heart failure. Sodium-glucose cotransporter 2 inhibitors and dipeptidyl peptidase-4 inhibitors reported to have positive CV outcomes; especially, combination therapy with dapagliflozin and sitagliptin seem to be suitable therapeutic option. However, data upon the fixed-dose combination of these agents is limited. This review discusses the rationale and clinical utility of combination therapy with dapagliflozin and sitagliptin in improving glycemic control and reducing cardiovascular events in patients with type 2 diabetes mellitus with multiple cardiovascular risk factors.
Keywords
Cardiovascular disease; Diabetes; Risk factors; Sodiumglucose cotransporter 2 inhibitors; Dipeptidyl peptidase-4 inhibitors; Dapagliflozin; Sitagliptin.
Article Details
1. Introduction
The incidence of type 2 diabetes mellitus (T2DM) is rapidly increasing often resulting in significant metabolic disorders and severe complications. Cardiovascular (CV) risk reduction in T2DM is of utmost importance in order to reduce the risk of CV morbidity and mortality[1]. Despite a variety of treatments currently available, cases of T2DM are uncontrolled which usually leads to serious health consequences such as impaired kidney function, blindness, stroke, myocardial infarction and lower limb amputation[2].
Several large randomized controlled trials with newer antihyperglycemic agents have demonstrated the cardiovascular safety along with reduction in cardiovascular outcomes[3]. In patients with T2DM with multiple risk factors, the role of combination therapy with sodium-glucose cotransporter 2 inhibitors and dipeptidyl peptidase-4 inhibitors in such clinical scenario need to be overviewed. This minireview discusses the rationale, evidence and clinical utility of combination therapy with dapagliflozin and sitagliptin in improving glycemic control and reducing adverse CV events in patients with T2DM with multiple CV risk factors.
1.1 Unmet Medical Need
Despite intensive glycaemia control having proven clinical benefits for several outcomes, the residual risk of cardiovascular (CV) death has remained a significant unmet need in patients with T2DM[4]. The Asian-Indian phenotype of T2DM is uniquely characterized for cardiometabolic risk. In the context of implementing patient-centric holistic cardio-metabolic risk management as a priority, the choice of various combinations of antidiabetic agents should be individualized [5].
|
Sr. No. |
Unmet Medical Need |
|
1 |
A need for a combinatorial approach to address multiple pathophysiological mechanisms of hyperglycemia to achieve robust glycemic control. |
|
2 |
A need for additional treatments that provide both glycemic and non-glycemic benefits, as the control of diabetes comorbidities is needed in most of the patients. |
|
3 |
Reducing the occurrence of hypoglycaemia or weight gain, as recurrent distressing side effects of traditional antidiabetic agents reduces the morale of not only the patient but also the treating physician. |
|
4 |
An oral treatment option that not only meets all of the pressing needs but additionally improves the compliance of the patients in need. |
Table 1: Key unmet medical needs in patients with type 2 diabetes mellitus with multiple cardiovascular risk factors[6].
1.2 Scope for Sodium-glucose cotransporter 2 inhibitors and dipeptidyl peptidase-4 inhibitors
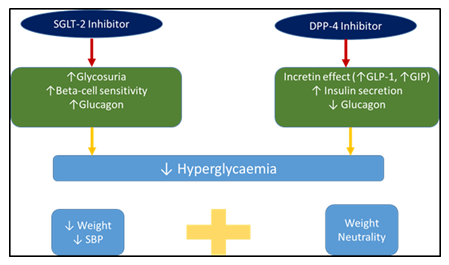
Dual therapy (initial combination or stepwise approach) is more potent than either monotherapy in patients treated with diet and exercise or already treated with metformin. Combining the two pharmacological options is safe and does not induce hypoglycemia. The additional glucose-lowering effect is more marked when a gliflozin is added to a gliptin than when a gliptin is added to a gliflozin [8]. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have demonstrated improved CV outcomes regardless of glycemia control; these agents now form an essential part of the armamentarium for appropriate cardiometabolic risk management in T2DM[7]. Combination therapy versus monotherapy shown to achieve glycaemic control in cases with uncontrolled hyperglycaemic status. Combined therapy with two specific classes of antidiabetic agents, namely, dipeptidyl peptidase 4 inhibitors (DPP4i) and SGLT2i target several pathophysiological pathways and been reported with certain cardiovascular benefits at various clinical studies[8].
The combined use of SGLT2i and DPP4i agents not only provides medications that complement each other well, but also targets at least six of the eight components in the ‘‘ominous octet’’. Hence after metformin initiation or even prior to metformin initiation in suitable patients (metformin contraindicated or intolerant), or in patients with high HbA1c who fail on metformin, this combination may give excellent clinical benefit(s) to the patients, thus facilitating the ‘‘treat early and treat right’’ approach [9].
Rationale for Use of Dapagliflozin and Sitagliptin
A ‘‘pathophysiological approach’’ using initial combination therapy with agents known to address the established defects in T2DM seems more rational. It is preferable to use combination therapies having complementary mechanisms of action that target different pathways addressing the multiple pathophysiologic abnormalities of T2DM[10]. Reported evidence with SGLT2i and several clinical trials of DPP4i have demonstrated that these agents reduce glycaemic variability in patients with T2DM. Both of these classes of medications are associated with lower risks for hypoglycemia[1].
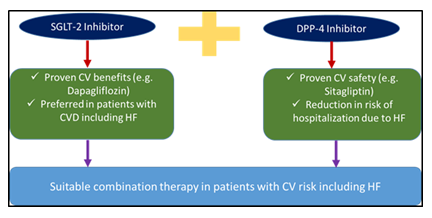
Fixed-dose combination (FDC) of SGLT2i and DPP4i is the unique non-metformin-based FDC been available in India[11]. After metformin initiation or even prior to metformin initiation in suitable patients (metformin contraindicated or intolerant), or in patients with high HbA1c who fail on metformin, this combination may give excellent clinical benefit(s) to the patients, thus facilitating the ‘‘treat early and treat right’’ approach. Below figure depicts the beneficial role of both these drugs in patients with diabetes and associated CV risk especially the risk of HF.
Cardiovascular outcome trials (CVOTs) have consistently shown that treatment with SGLT2i reduces hospitalization for heart failure (HHF) and secondary renal outcomes in terms of incident or worsening nephropathy in patients with T2DM and CV disease[12]. Also, with respect to the primary endpoint (3PMACE), the CV safety profile of Sitagliptin was established in the CVOT like TECOS study (Trial Evaluating Cardiovascular Outcomes with Sitagliptin). TECOS study clearly established the fact that, In T2DM and established CVD, adding sitagliptin to usual care offers favourable CV outcomes[13].This combination seems to be rationale to use in patient with HF with respect to the recommendations as depicted at figure 2.
1.3 Evidence for Dapagliflozin and Sitagliptin
Unlike oral antidiabetic drugs from several other classes, the efficacy of dapagliflozin is independent of insulin secretion and action. When used in combination with other antidiabetic drugs, dapagliflozin provides complementary therapy via its unique mechanism of action[14].
Sitagliptin works to competitively inhibit the enzyme dipeptidyl peptidase 4 (DPP-4). This enzyme breaks down the incretins GLP-1 and GIP, gastrointestinal hormones released in response to a meal. By preventing breakdown of GLP-1 and GIP, they are able to increase the secretion of insulin and suppress the release of glucagon by the alpha cells of the pancreas. This drives blood glucose levels towards normal. As the blood glucose level approaches normal, the amounts of insulin released and glucagon suppressed diminishes, thus tending to prevent an "overshoot" and subsequent low blood sugar (hypoglycemia), which is seen with some other oral hypoglycemic agents[15].
Sitagliptin has been shown to lower HbA1c level by about 0.7% points versus placebo. It does not cause weight gain and has less hypoglycemia compared to sulfonylureas. Sitagliptin is recommended as a second-line drug (in combination with other drugs) after the combination of diet/exercise and metformin fails[16]. Dapagliflozin added to Sitagliptin been reported to have additional clinical benefit and demonstrated well tolerated profile in patients with inadequately controlled T2DM [17].
Reported clinical evidence suggest utility of fixed-dose combination of Dapagliflozin and Sitagliptin shown to be effective in uncontrolled T2DM or T2DM with multiple cardiovascular risk factors. Dapagliflozin reported to be effective as add-on therapy to sitagliptin with or without metformin in a 24-week, multicenter, randomized, double-blind, placebo-controlled study. As reported, in patients with type 2 diabetes, inadequately controlled on sitagliptin with or without metformin, add-on treatment with dapagliflozin provides additional clinical benefit with well tolerability. Around 432 patients were randomized in the study to receive dapagliflozin 10 mg/day or placebo added to sitagliptin (100 mg/day) ± metformin (≥1,500 mg/day). In this trial, baseline HbA1c and FPG levels were 7.9% (63.0 mmol/mol) and 162.2 mg/dL (9.0 mmol/L) for the dapagliflozin group and 8.0% (64.0 mmol/mol) and 163 mg/dL (9.0 mmol/L) for placebo. At week 24, dapagliflozin significantly reduced mean HbA1c levels (-0.5% [-4.9 mmol/mol]) versus placebo (0.0% [+0.4 mmol/mol]). Dapagliflozin reduced body weight versus placebo (-2.1 and -0.3 kg) and reduced HbA1c levels in patients with baseline values ≥8.0% (-0.8% [8.7 mmol/mol] and 0.0% [0.3 mmol/mol]) and fasting plasma glucose levels (-24.1 mg/dL [-1.3 mmol/L] and 3.8 mg/dL [0.2 mmol/L]). Similar results were observed when data were stratified by background therapy. Glycemic and weight benefits observed at week 24 were maintained through week 48. Changes from baseline in systolic blood pressure at week 8 were not significantly different between treatment groups. Over 48 weeks, fewer patients receiving dapagliflozin were discontinued or rescued for failing to achieve glycemic targets compared with placebo. Adverse events were balanced between groups, and discontinuation rates were low. At week 48, signs and symptoms suggestive of genital infection were more frequent with dapagliflozin (9.8%) than with placebo (0.4%). Signs and symptoms suggestive of urinary tract infection were balanced between dapagliflozin (6.7%) and placebo (6.2%) [17].
The wide ranging clinical outcomes associated with this combination, including improvement of glycemia and adiposity, reduction of metabolic and vascular risk, safety, and simplicity for sustainable compliance, are extremely relevant to the Asian Indian patient population living with T2DM. Early intensive therapeutic control has proven benefits in clinical outcomes. This FDC likely to be beneficial clinically in given condition. In addition to reducing pill burden and improving compliance, given combination therapy with two drugs may help patients achieve their target HbA1c faster than monotherapy. Dapagliflozin and Sitagliptin has a potential to be an essential part of the available armamentarium for appropriate cardiometabolic risk management in T2DM.
2. Summary
Medications with good glycaemic efficacy, low risk of hypoglycemia and weight loss help to intensify the treatment without introducing common adverse events, such as hypoglycaemia and weight gain. These advantages may help overcome clinical inertia for treatment intensification. Targeting multiple pathophysiological pathways for T2DM with Dapagliflozin and Sitagliptin combination therapy seem to be a clear benefit including certain extraglycemic benefits as it helps to reduce body weight and blood pressure suggesting for the use of this combination early in T2DM management.
3. Conclusion
Dapagliflozin and sitagliptin forms an essential part of the current armamentarium for appropriate cardiometabolic risk management in T2DM which seem to be safer,shown to achieve rapidand sustained glycemic control especially associated with improvement in both insulin resistance and beta cell function.
Disclaimer:
None
References
- Joseph JJ, Deedwania P, Acharya T, et al. American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Hypertension. Comprehensive Management of Cardiovascular Risk Factors for Adults with Type 2 Diabetes: A Scientific Statement from the American Heart Association. Circulation 145(9)(2022): e722-e759.
- Iatcu CO, Steen A, Covasa M. Gut Microbiota and Complications of Type-2 Diabetes. Nutrients 14(1)(2021): 166.
- Lo CWH, Fei Y, Cheung BMY. Cardiovascular Outcomes in Trials of New Antidiabetic Drug Classes. Card Fail Rev 5(2021): e04.
- Giugliano D, Maiorino MI, Bellastella G, et al. Glycemic Control, Preexisting Cardiovascular Disease, and Risk of Major Cardiovascular Events in Patients with Type 2 Diabetes Mellitus: Systematic Review with Meta-Analysis of Cardiovascular Outcome Trials and Intensive Glucose Control Trials. J Am Heart Assoc 8(12)(2019): e012356.
- Wolf RM, Nagpal M, Magge SN. Diabetes and cardiometabolic risk in South Asian youth: A review. Pediatr Diabetes 22(1)(2021): 52-66.
- Chadha M, Das AK, Deb P, et al. Expert Opinion: Optimum Clinical Approach to Combination-Use of SGLT2i + DPP4i in the Indian Diabetes Setting. Diabetes Ther 13(5)(2022): 1097-1114.
- Ali A, Bain S, Hicks D, et al.As part of The Improving Diabetes Steering Committee. SGLT2 Inhibitors: Cardiovascular Benefits Beyond HbA1c-Translating Evidence into Practice. Diabetes Ther 10(5) (2019): 1595-1622.
- Scheen AJ. DPP-4 inhibitor plus SGLT-2 inhibitor as combination therapy for type 2 diabetes: from rationale to clinical aspects. Expert Opin Drug Metab Toxicol 12(12)(2016): 1407-1417.
- Kim ES, Deeks ED. Empagliflozin/Linagliptin: A Review in Type 2 Diabetes. Drugs 75(13)(2015): 1547-57.
- Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383(9922)(2014): 1068-83.
- Li D, Shi W, Wang T, et al. SGLT2 inhibitor plus DPP-4 inhibitor as combination therapy for type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes Metab 20(8)(2018): 1972-1976.
- Gronda EG, Vanoli E, Iacoviello M, et al. Renal effects of SGLT2 inhibitors in cardiovascular patients with and without chronic kidney disease: focus on heart failure and renal outcomes. Heart Fail Rev 31(2022): 1–10.
- Green JB, Bethel MA, Armstrong PW, et al. TECOS Study Group. Effect of Sitagliptin on Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 373(3)(2015): 232-42.
- Dhillon S. Dapagliflozin: A Review in Type 2 Diabetes. Drugs 79(10) (2019): 1135-1146.
- Deacon CF. Physiology and Pharmacology of DPP-4 in Glucose Homeostasis and the Treatment of Type 2 Diabetes. Front Endocrinol (Lausanne) 15(2019): 10:80.
- St Onge EL, Miller S, Clements E. Sitagliptin/Metformin (janumet) as combination therapy in the treatment of type-2 diabetes mellitus. P T 37(12)(2012): 699-708.
- Jabbour SA, Hardy E, Sugg J, et al. Study 10 Group. Dapagliflozin is effective as add-on therapy to sitagliptin with or without metformin: a 24-week, multicenter, randomized, double-blind, placebo-controlled study. Diabetes Care 37(3)(2014): 740-50.