Coronasomnia: A Hidden Problem of the COVID era. Is Melatonin a Potential Solution?
Article Information
Rashmi Supriya1,2*, Kumar Purnendu Singh3*, Frederic Dutheil4, Yaodong Gu1, Julien S Baker1,2
1Faculty of Sports Science, Ningbo University, Zhejiang, 315211, China.
2Centre for Health and Exercise Science Research, Department of Sport, Physical Education and Health, Hong Kong Baptist University, Kowloon Tong, 999077, Hong Kong.
3FEBT, School of Environment, Resources and Development, Asian Institute of Technology, Paholyothin Highway, Klong Luang, Pathum Thani 12120, Thailand
4University Clermont Auvergne, CNRS, LaPSCo, Physiological and Psychosocial Stress, CHU Clermont-Ferrand, University Hospital of Clermont-Ferrand, Preventive and Occupational Medicine, Witty Fit, F-63000 Clermont-Ferrand, France
*Corresponding Author 1: Rashmi Supriya, Centre for Health and Exercise Science Research, Department of Sport, Physical Education and Health, Hong Kong Baptist University, Kowloon Tong, 999077, Hong Kong.
*Corresponding Author 2: Kumar Purnendu Singh, FEBT, School of Environment, Resources and Development, Asian Institute of Technology, Paholyothin Highway, Klong Luang, Pathum Thani 12120, Thailand
Received: 17 February 2022; Accepted: 25 February 2022; Published: 28 February 2022
Citation:
Rashmi Supriya, Kumar Purnendu Singh, Frederic Dutheil, Yaodong Gu, Julien S Baker. Coronasomnia: A Hidden Problem of the COVID era. Is Melatonin a Potential Solution?. Journal of Food Science and Nutrition Research 5 (2022): 325-340.
Share at FacebookAbstract
Globally, changes in work cultures have impacted on all life, and individuals have reported increased insomnia “Coronasomnia” as a result of COVID-19. Correct nutrition, in relation to micronutrient concentration, may have beneficial effects in controlling our biological sleep clocks. Specifically, melatonin supplementaions are being recommended for the COVID generation. However, there have been mixed reports regarding melatonin supplementation using high dosages for certain population groups, and there may be disadvantages in using melatonin as an exogenous supplement (oral tablet or injectable drug) in the long term. As a result, melatonin may not be suitable for all post COVID generations without further clinical trials. However, melatonin as a dietary supplement could have significant health benefits without causing any adverse effects. Therefore, the main aim of this opinion article is to highlight the challenges of “Coronasomnia” related to COVID 19, which has been overlooked. In addition, we highlight the research need for clinical trials on melatonin supplementation for inclusion in the diets of the COVID generation. Supplementation regimes using naturally occurring melatonin obtained from dietary sources will regulate central biological cycle naturally. Consequently, future research is needed to investigate whether melatonin containing foods are clinically beneficial to the COVID generation by increasing the bioavailability of melatonin using dietary supplementation.
Keywords
Coronasomnia, Covidsomnia, Melatonin, Diet, Work culture
Coronasomnia articles; Covidsomnia articles; Melatonin articles; Diet articles; Work culture articles
Coronasomnia articles Coronasomnia Research articles Coronasomnia review articles Coronasomnia PubMed articles Coronasomnia PubMed Central articles Coronasomnia 2023 articles Coronasomnia 2024 articles Coronasomnia Scopus articles Coronasomnia impact factor journals Coronasomnia Scopus journals Coronasomnia PubMed journals Coronasomnia medical journals Coronasomnia free journals Coronasomnia best journals Coronasomnia top journals Coronasomnia free medical journals Coronasomnia famous journals Coronasomnia Google Scholar indexed journals Covidsomnia articles Covidsomnia Research articles Covidsomnia review articles Covidsomnia PubMed articles Covidsomnia PubMed Central articles Covidsomnia 2023 articles Covidsomnia 2024 articles Covidsomnia Scopus articles Covidsomnia impact factor journals Covidsomnia Scopus journals Covidsomnia PubMed journals Covidsomnia medical journals Covidsomnia free journals Covidsomnia best journals Covidsomnia top journals Covidsomnia free medical journals Covidsomnia famous journals Covidsomnia Google Scholar indexed journals Melatonin articles Melatonin Research articles Melatonin review articles Melatonin PubMed articles Melatonin PubMed Central articles Melatonin 2023 articles Melatonin 2024 articles Melatonin Scopus articles Melatonin impact factor journals Melatonin Scopus journals Melatonin PubMed journals Melatonin medical journals Melatonin free journals Melatonin best journals Melatonin top journals Melatonin free medical journals Melatonin famous journals Melatonin Google Scholar indexed journals Diet articles Diet Research articles Diet review articles Diet PubMed articles Diet PubMed Central articles Diet 2023 articles Diet 2024 articles Diet Scopus articles Diet impact factor journals Diet Scopus journals Diet PubMed journals Diet medical journals Diet free journals Diet best journals Diet top journals Diet free medical journals Diet famous journals Diet Google Scholar indexed journals Work culture articles Work culture Research articles Work culture review articles Work culture PubMed articles Work culture PubMed Central articles Work culture 2023 articles Work culture 2024 articles Work culture Scopus articles Work culture impact factor journals Work culture Scopus journals Work culture PubMed journals Work culture medical journals Work culture free journals Work culture best journals Work culture top journals Work culture free medical journals Work culture famous journals Work culture Google Scholar indexed journals dietary supplementation articles dietary supplementation Research articles dietary supplementation review articles dietary supplementation PubMed articles dietary supplementation PubMed Central articles dietary supplementation 2023 articles dietary supplementation 2024 articles dietary supplementation Scopus articles dietary supplementation impact factor journals dietary supplementation Scopus journals dietary supplementation PubMed journals dietary supplementation medical journals dietary supplementation free journals dietary supplementation best journals dietary supplementation top journals dietary supplementation free medical journals dietary supplementation famous journals dietary supplementation Google Scholar indexed journals nutritional components articles nutritional components Research articles nutritional components review articles nutritional components PubMed articles nutritional components PubMed Central articles nutritional components 2023 articles nutritional components 2024 articles nutritional components Scopus articles nutritional components impact factor journals nutritional components Scopus journals nutritional components PubMed journals nutritional components medical journals nutritional components free journals nutritional components best journals nutritional components top journals nutritional components free medical journals nutritional components famous journals nutritional components Google Scholar indexed journals biological cycles articles biological cycles Research articles biological cycles review articles biological cycles PubMed articles biological cycles PubMed Central articles biological cycles 2023 articles biological cycles 2024 articles biological cycles Scopus articles biological cycles impact factor journals biological cycles Scopus journals biological cycles PubMed journals biological cycles medical journals biological cycles free journals biological cycles best journals biological cycles top journals biological cycles free medical journals biological cycles famous journals biological cycles Google Scholar indexed journals food source articles food source Research articles food source review articles food source PubMed articles food source PubMed Central articles food source 2023 articles food source 2024 articles food source Scopus articles food source impact factor journals food source Scopus journals food source PubMed journals food source medical journals food source free journals food source best journals food source top journals food source free medical journals food source famous journals food source Google Scholar indexed journals
Article Details
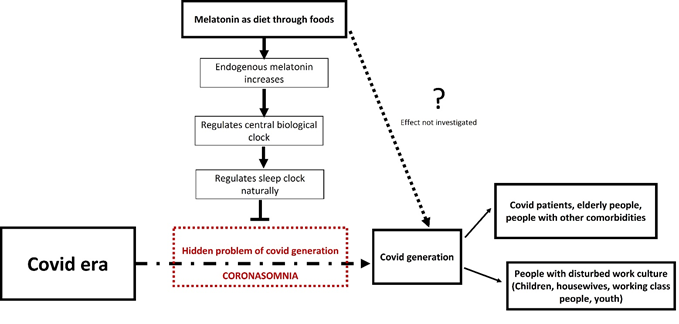
Graphical Abstract
1. Introduction
The term “Coronasomnia”, refers to sleep disorders caused by stress, anxiety and depression linked to the COVID-19 pandemic [1,2]. The present time of uncertainty and constant barrage of information due to the pandemic has led to disruptions in our daily routines, activity levels and work cultures. These changes have ultimately led to increased sleep disturbances [3]. Confinement at home, homeschooling, avoiding large gatherings in public places, wearing a mask, not being able to perform 'normal' activities, loneliness, economic hardship, juggling work and school, and parenting challenges, have all increased stress, anxiety, and depression levels during the pandemic. All the above have been implicated as causes for increases in insomnia post COVID-19 [4]. The change in our work cultures has affected us all, and has resulted in some homes becoming workplaces. This has had further effects on individuals at home who are not employed, resulting in an increase in insomnia prevalence worldwide. All sections of the population are affected by the disruption to daily routines and work cultures, including women, young people, adolescents, and children. Nutrition plays a crucial role in sleep wellness. Improving sleep with dietary management is an easy, convenient, and inexpensive solution to insomnia. Experimental studies have shown that certain nutritional components, or their metabolites, may have beneficial effects in controlling our biological sleep clocks [5]. The administration of melatonin, magnesium, and zinc at night appears to show positive results in improving the quality of sleep and quality of life in long-term care facility residents who suffer from primary insomnia [6]. Specifically, melatonin has been shown to limit virus-related disease transmission and may also benefit COVID-19 patients. Patients with COVID-19 might benefit from melatonin's ability to reduce blood vessel permeability, anxiety, use of sedation, and improve sleep quality, all of which may also lead to improved clinical outcomes. This speculation needs further confirmation by additional experimental and clinical studies [7]. Studies have suggested, considering melatonin as a prophylactic treatment or a complementary therapy. The Multiple actions of melatonin as a treatment for inflammation, oxidation, and viral infections make it an excellent choice for use. A large dose of melatonin, alone or in combination with currently recommended drugs, such as hydroxychloroquine and chloroquine, has been suggested for use under clinical conditions [8]. Aside from being readily available, readily synthesizable in large quantities, inexpensive, melatonin can be easily self-administered. However, it is important to note that melatonin is regulated as a dietary supplement in the United States and Canada, and not in other countries. This means it has fewer regulations than prescription medicines recognized by the Food and Drug Administration (FDA). In addition, melatonin packaging does not provide ingredient information [9]. Further to this, melatonin is only available with a prescription in several other countries [10]. Melatonin does not have a recommended dietary allowance and should contain a dosage of 0.5 to 3 milligrams for sleep-related issues, according to some experts. Higher doses may result in drowsiness and many long-term side effects for certain individuals. There have been mixed reports regarding melatonin supplementation using high dosages. There are also limitations for many population groups including pregnant women, children, and asthma patients, and as a result, melatonin may not be suitable for certain post COVID generations without further clinical trials. In contrast to this, the benefits of supplementing with melatonin using dietary interventions have not been examined, specifically for COVID populations and vulnerable patients, such as those with underlying comorbidities. Remarkably, researchers have suggested that using melatonin as a dietary supplement could have beneficial effects without causing any adverse reactions. Melatonin does not cause any adverse effects when consumed as a food or drink. In addition, a 28-day randomized, double-blind clinical trial of 10 mg melatonin (orally) found no toxicological effects at a dose of 1-10 mg/kg [11,12] Moreover, high-dose melatonin had no toxic effects in pregnant animal models [10,13]. Recent studies indicated that melatonin improves sleep efficiency and melatonin-rich foods could improve sleep quality. The level of melatonin in the serum of humans can increase significantly after eating foods containing melatonin. Further, studies have shown that melatonin exhibits many bioactive properties, including antioxidant activity, anti-inflammatory characteristics, immunity boosting effects, anticancer activity, cardiovascular protection, and anti-diabetic, anti-obese, and anti-aging properties which are all associated with coronasomnia [10]. The suprachiasmatic nucleus (SCN) is responsible for many functions in the body including the daily sleep-wake cycle, body temperature and hormone production, including increases in growth hormone. Part of the role of growth hormone is to repair and restore processes in the body. The SCN regulates the timing of melatonin release, while melatonin feeds back to the SCN to decrease SCN neuronal firing [14,15]. Interestingly, in the animal model it has been suggested that endogenous melatonin could sustain circadian rhythmicity and the phase relationship between the molecular partners of the SCN circadian system on a long-term basis [16]. In the COVID era, coronasomnia is not simply a sleep condition that can be cured by taking a single medication. Coronasomnia is due to a disturbed biological clock. Resetting the body's biological clock requires addressing problems associated with the endocrine system and is more challenging than just recalibrating the clock. The purpose of this article is to highlight the challenges of “Coronasomnia” related to COVID 19, which has been overlooked. Therefore, our aim is not to minimize the importance of exogenous melatonin as an adjuvant therapy for COVID sufferers, including those with chronic diseases, but to highlight the research gap in clinical trials on melatonin supplementation in the diets of COVID-19 generations. We suggest here that melatonin as an exogenous supplement (oral tablet or injectable drug) could have hidden disadvantages (that need exploration) in the long term and hence, should be substituted with natural melatonin as a food source that will not only regulate sleep cycles, but will also regulate biological cycles. Bioavailability of melatonin is low in natural food sources, but is safe compared to high dosages contained in artificial supplements. Consequently, we suggest that there is an urgent need for research to investigate methods to increase the bioavailability of melatonin through food supplements and to examine whether melatonin containing foods are clinically beneficial for the COVID generation.
2. Coronasomnia
In 2020, the keyword "insomnia" was googled more frequently than recorded previously. As a result of the stress of COVID-19, individuals globally experienced increased insomnia. In a study published in the American Academy of Sleep Medicine, there were 2.77 million Google searches for "insomnia" during the first five months of 2020, an increase of 58% over the prior period. It is even referred to as 'Coronasomnia' or 'Covid-somnia' by some experts [17,18]. Coronasomnia, is a term used to describe sleep disorders caused by stress resulting from the COVID-19 pandemic. During the pandemic, a study revealed very high rates of clinically significant insomnia (20%), acute stress (15.8%), anxiety (18.5%), and depression (24.5%). Four groups of respondents were classified based on their level of exposure and threat of COVID-19 infection. Participants living near the epicenter (Hubei province) and those who experienced higher degrees of panic, such as health care professionals and management workers, reported more severe insomnia and psychological symptoms [19]. Individual daily routines and level of activity were disrupted by the virus, and many people have probably experienced a reduction in sleep as a result. Having to isolate at home, homeschooling, avoid large gatherings in public places, wearing a mask, and not being able to participate in 'normal' activities contributed to the experiences. It is also true that stress levels increased during the flu pandemic due to many similar factors, including loneliness, economic hardships, juggling work and school, and parenting challenges. In addition, being isolated can impact on individual sleep patterns. Stress impacts all parts of our lives, so it is inevitable that it will affect how we sleep. Research has identified that staying at home can disrupt wakefulness cues associated with light. Circadian rhythms are organized based on exposure to sunlight. As many of us still work from home, some individuals may sleep late and have different schedules. This can contribute to insomnia by disrupting sleep patterns and making sleeping more difficult the following night. Coronasomnia impacts are extremely serious. Stress and lack of sleep can have a negative impact on our overall health and endocrine system. Chronic sleep deprivation lowers our immunity and makes us more susceptible to viruses and decreases our cognitive abilities. A chronic lack of sleep can affect the entire body, leading to worsening cardiovascular and metabolic conditions, including a higher risk of weight gain, diabetes, and high blood pressure [18] (Figure 1).
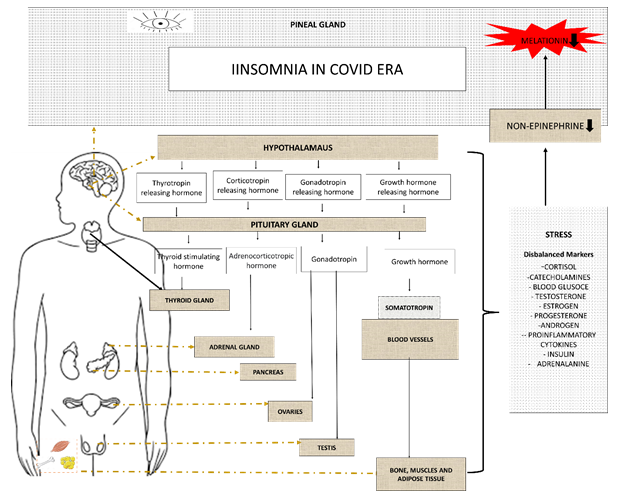
Figure 1: Coronasomnia as result of disbalance of hormones due to stress. Stressed endocrine organs release stress biomolecules that reduce nor-epinephrine and melatonin levels in the pineal gland.
3. Pre and post covid Insomnia
The COVID-19 pandemic was associated with the highest levels of stress, anxiety, and depression in individuals with post-pandemic insomnia symptoms. This was in comparison with those without insomnia symptoms or those with pre-existing insomnia symptoms. It was noted that this pattern of results was observed for individuals with and without a psychological condition diagnosis, with only small differences across countries. Therefore, insomnia symptoms following the COVID-19 pandemic may be a sign of poor mental health [20]. As a result of the COVID-19 pandemic, many aspects of our lives have changed in a profound way. Several surveys conducted in various countries have found that healthcare workers [1,2] and general population [3-6] have high rates of sleep problems (insomnia) and psychological problems (such as anxiety and depression), as well as changes in sleep scheduling factors. A study among 594 adults (mean age: 48.3 ± 13.1 years; 64.0% women) reported an overall 26.7% increase in insomnia rates. According to the findings, the higher prevalence in 2020 may be attributable to higher levels of sub-syndrome insomnia (25% to 32%) while the prevalence of the syndrome increased only from 16.8% to 19%. A significant association between sleep and psychological symptoms, being in confinement, lower social support, living alone, increased time using electronic devices, higher financial stress and reduced physical exercise has also been reported [21]. The prevalence of insomnia varies between 10% and 40%, depending on whether it is viewed as a disorder (5-10% prevalence) or a symptom (30% prevalence) [22]. Following the pandemic, the prevalence rate increased. In a study published in 2021, the number of individuals suffering from insomnia increased from 1 in 6 to 1 in 4 in the United Kingdom, while the number of individuals suffering from insomnia in China increasing from 14.6% to 20% during peak lockdown periods.
4. Is change in work culture the main cause of Coronasomnia?
Social restrictions implemented in almost all countries to combat the outbreak have resulted in unemployment, financial hardships, and a lower quality of life for many people [4], a situation that has seriously affected their lives and jobs [4]. Work culture has impacted every one’s life and has led to increased insomnia worldwide. The disruption in daily routines and work culture is affecting all sections of people including women, youth, adolescents, and children. Housewives saw their work increase exponentially. Previously, housewives could at least get some respite while the spouse worked, or the children were in school. In the case of children studying videos and mail, the parents - especially the homemakers had to act as teachers to help the younger children with online and computer aided teaching. This added to the homemaker's workload and increased stress [23]. The impact of COVID-19 on women was greater than that of any other member of the family in terms of psychological, economic, familial, and societal impact. As a result, tasks such as caring for patients, disinfecting the environment and equipment, paying attention to nutrition, maintaining family relationships, caring for children's education, and maintaining emotional and marital relationships were all additional demands on housewives during quarantine [24]. In the case of adults or working youths, new research conducted during the pandemic revealed that home-working workers in the United Kingdom, Austria, Canada, and the United States are actively working for more hours per day than the hours recorded prior to the pandemic. As a result of home-based working, the average working hours a day in those countries increased by 2.5. Another finding suggested that 55% of UK employees say they were asked to work outside their regular hours, and 74% say they have suffered fatigue, stress, or burnout. 44% of employees reported increasing workloads after working from home during the pandemic; 31% reported feeling depressed, anxious, or exhausted. "People's jobs are becoming ever more blurred with their personal lives at a time when it's important to maintain a clear separation between the two" [25]. Children’s work cultures have also been disturbed. During the COVID-19 pandemic, sleep problems in children and adolescents have been alarming. The proportion of children whose sleep quality deteriorated during the pandemic was nearly three times that of those whose sleep quality improved. During the pandemic, nearly half of healthy children did not meet sleep duration recommendations [26]. The altered sleep patterns of children and adolescents as well as the adult population can be attributed to two major factors: i) the increased stress and anxiety associated with COVID-19 infection [27] ii) the increased use of media and screens as a result of the reduced opportunity for alternative activities [28,29]. According to a survey, 70% of children under 16 were going to bed later - and waking up later (57%). In the study, nearly three quarters (74%) of parents said that during the Coronavirus lockdown, their children were relying more heavily on technology. It was found that teenagers often attempted to enforce sleep patterns that were not natural biologically. While society and school force them to get up earlier, lockdown lets them drift away from their usual sleep patterns [30].
5. Dietetics may play an important role
Sleep wellness is strongly linked to nutrition. Managing a diet to improve sleep is an effective, convenient, and inexpensive method. Experimentally, some nutritional components or their metabolites have been shown to be beneficial. In long-term care facility residents with primary insomnia, taking melatonin, magnesium, and zinc nightly improved sleep quality and quality of life [6]. However, sleep and nutrition interact in a complicated way. Due to the complex composition of food, as well as individual absorption and metabolic abilities, the relationship between the consumption of a particular food and sleep wellness is more complicated. There is a lack of solid scientific evidence related to the benefits and most of the information is hypothetical. There are many observational or cross-sectional studies using limited sample sizes and the results are often conflicting. To further confirm the role of dietary nutrition in sleep wellness, more high-quality cohort studies and randomized controlled trials are needed. A better animal model to mimic clinical situations is also of great importance.
6. Perplexity of melatonin supplements in the COVID era
Research suggests that melatonin may be useful in the treatment of COVID-19. In the light of the lack of clinical data, researchers propose the use of melatonin to reduce morbidity and mortality in patients with COVID-19 [7,8,31]. Melatonin may be a helpful treatment for sleep disturbances related to COVID-19 due to its role in circadian sleep rhythm and the lack of adverse effects on respiratory function. A review article describes melatonin's effects other than its sleep-related effects, which makes it a viable therapeutic option for patients with COVID-19. Preclinical data indicate that melatonin may slow COVID-19 progression. There is a possibility that it might reduce the risk of SARS-CoV-2 entering cells, reduce hyper-inflammation and the activation of immune cells, limit the damage caused by free radicals to tissues, as well as reduce ventilator-induced lung injury and the risk of disability from fibrotic changes within lung tissue. COVID-19 vaccination may also be enhanced by melatonin. As a result of its high safety profile and potential anti-SARS-CoV-2 effects, melatonin is a promising treatment for COVID-19 patients experiencing sleep disturbances [31]. Nevertheless, randomized clinical trials are needed to prove that melatonin is effective in treating COVID-19. There is a suggestion that taking a melatonin pill is safe and effective for getting better sleep. There is a problem with this example since melatonin is a hormone, not a vitamin. Melatonin supplements work in the exact same way as other hormone therapies (estrogen, testosterone), by introducing a biochemical into the body to cause physiological changes. As a matter of fact, melatonin is available as an over-the-counter supplement only in the United States and Canada. Other places require prescriptions. Hence, it's not regulated the same way as a pharmaceutical medication would be in terms of consistent quality and dosage. Synthetic melatonin has the disadvantage of not instantly providing a sleep state. In other words, it's a chemical signal for our bodies to shut down for the day, setting off a series of physiological events. It affects more than our sleep mechanisms when we increase our melatonin levels. It can affect our digestion and mood. One of the biggest problems with taking this hormone in synthetic form is that it interferes with our body's natural melatonin production. It has been found that taking melatonin at the wrong time or taking too much can desensitize our melatonin receptors, which can permanently disable our ability to use melatonin. Melatonin supplementation is not likely to help our underlying sleep problems. Melatonin won't help if our sleep problem is anxiety-stress-or gut-related. Moreover, it can't make up for any other sleep-disturbing habits we have developed [32]. Melatonin should be administered at appropriate times, especially during chronic treatment. The melatonin profile is highly variable between individuals; however, a person's profile is reasonably reproducible from one day to the next. Additionally, individual differences in the absorption, metabolism, and excretion of melatonin must be considered if desired clinical efficacy is to be achieved [33]. Melatonin sensitivity and pharmacokinetics are different between individuals, and a dose of 0.3-0.5 mg may prove more effective than a higher dose in some subjects. A consensus of opinion is lacking regarding dosage. Different formulations of doses are available, and the dose formulation used varies among clinical application [34]. The majority of clinical trials and studies involving melatonin report that this drug is generally safe and does not cause toxic side effects when tested using the usual doses from 0.5 to 5 mg/d [5]. In chronic melatonin treatment, dosage may need to be changed depending on the season; further studies are needed to determine whether or not melatonin suppression will have adverse long-term effects [35]. Melatonin sleep supplements should be used wisely and safely. Generally, melatonin is not suitable for people with allergies. Before using this medication, individuals should consult the healthcare provider. This medication may not be suitable if individuals have certain medical conditions, such as diabetes, depression, bleeding, or a blood clotting disorder like hemophilia. Without medical advice pregnant women can’t use this product. This supplement may affect ovulation, making it difficult for women to become pregnant when taken in high doses. In contrast to many sleep medications, melatonin does not cause dependence, a diminished response following repeated use (habituation), or a hangover effect. Melatonin side effects include headache, nausea, and drowsiness. It can also cause short-lasting feelings of depression, mild tremor, mild anxiety, abdominal cramps, irritability, reduced alertness, confusion, and low blood pressure (hypotension) (Figure 2).
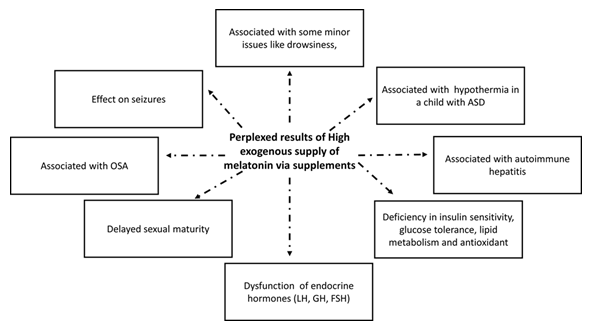
Figure 2: Perplexed results of high exogenous melatonin via supplements. OSA (Obstructive sleep Apnea), ASD (Autism Spectrum Disorder), LH (Luteinizing hormone), GH (Growth hormone) FSH (Follicle stimulating hormone).
Melatonin supplements can also interact with various medications, such as anticoagulants and antiplatelet medications, anticonvulsants, contraceptives, and diabetes medications [36-38]. There have been mixed reports regarding melatonin supplementation with high doses and these are also limited for many population groups including pregnant women, children, and asthma patients. As a result, melatonin may not be suitable for certain COVID populations without clinical trials.
7. Is Melatonin in the diet a solution for insomnia in the COVID era?
Almost all the body's organs produce melatonin from tryptophan, since the mitochondria are responsible for its production [39]. Melatonin plays an important role in health and aging. The anti-inflammatory, antiapoptotic, immunomodulatory, and powerful antioxidant properties of melatonin make it a potential adjunctive therapy for viral infections [39]. There are natural diet alternatives that can help ease our transition back into regular sleep patterns instead of over-the-counter sleep aids. A pill is never going to be the one solution to health dilemmas, so individuals should combine these foods with physical activity and a healthy sleep schedule. Almost all life forms, from prokaryotes to eukaryotes, have evolved their own circadian clocks as a result of the regular 24-hour rotation of the earth [40]. A master endogenous clock is found in the brain of mammals, including humans. In the premodern era, the timing of feeding and fasting cycles matched the patterns of daily wakefulness and sleep that correlated with the length of daylight and darkness. A circadian clock in our brain helps to coordinate and anticipate our behavior and metabolism in response to this environmental periodicity, which is caused by the earth's rotation. A number of input signals have been shown to ensure proper entrainment of the endogenous clock mechanism to the outside world, of which light, food intake and locomotor activity are the most significant [41]. We all have different sleep and wake patterns, but what causes these differences? Is it our lifestyle routine or is it something else? Nature does not manipulate our sleep-wake patterns at random. The suprachiasmatic nucleus (SCN) in the brain regulates a variety of body functions such as temperature, metabolism, and even hormone release. Living organisms possess their own internal biological clocks, also known as circadian rhythms. It has been identified that a specific nucleus in the hypothalamus regulates the timing of circadian rhythms. This specific nucleus is called the SCN. The SCN regulates many bodily functions, including sleep-wake cycles, body temperature, and growth hormone production, which aids in body repair and restoration. There is a significant role for melatonin in regulating sleep and other activities in the body. In response to the environmental light-dark cycle, the suprachiasmatic nucleus regulates the pineal gland's production of melatonin. Melatonin tells all the tissues in the body the time of day and the season. Sleep disorders associated with aging and different degenerative and developmental disorders are related to abnormalities in the circadian control of melatonin secretion. SCN control the timing of melatonin release, while melatonin decreases SCN neuronal firing [14]. Animal study research suggests that endogenous melatonin could sustain the phase relationship between the molecular partners of the SCN circadian system on a long-term basis [16,42] (Figure 3).
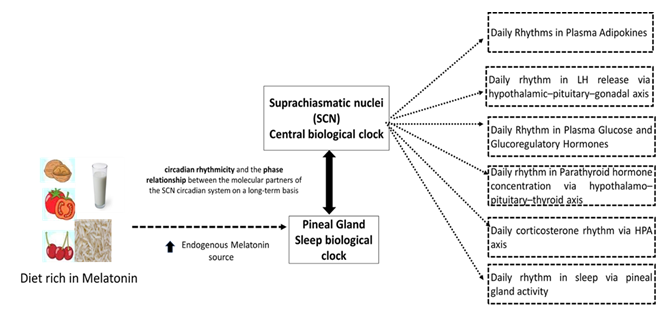
Figure 3: Long-term effect of endogenous melatonin may be to preserve the circadian rhythmicity and phase relationship between the suprachiasmatic nucleus circadian partners including daily rhythms in plasma adipokines, LH release, plasma glucose and glucoregulatory hormones, parathyroid hormones concentration, corticosterone and sleep. LH is Luteinizing hormone.
Melatonin in food and beverages has not been observed to have any adverse effects. A dose of 10 mg melatonin (orally) in a 28-day randomized, double-blind clinical trial found no toxicological effects [11,12]. Moreover, high-dose melatonin had no toxic effects in pregnant animal models [13,38]. Recent studies indicated that melatonin improves sleep efficiency and melatonin-rich foods could improve sleep quality. Concentrations in human blood have been shown to increase dramatically after consumption of foods containing melatonin [43,44]. Further, studies have shown that melatonin exhibits many bioactive properties, including antioxidant activity, anti-inflammatory characteristics, immunity boosting, anticancer activity, cardiovascular protection, anti-diabetic, anti-obese, and anti-aging properties [38]. Increasing dietary consumption of melatonin could be beneficial after childhood since its secretion decreases. The studies found that consumption of melatonin-rich foods increased the levels of circulating melatonin [45-47]. For instance, when rats were fed walnuts (Juglans regia L.) with melatonin concentrations of 3.5 ± 1.0 ng/g, there was an increase in blood melatonin levels and total antioxidant capacity, suggesting walnuts are a good source of melatonin [48]. In a study conducted on young, middle-aged and elderly participants (20 ± 10-year old, 45 ± 10-year old and 75 ± 10-year old, respectively), a significant increase in total antioxidant capacity, determined by total antioxidant capacity analysis, was observed in all three groups following the intake of grape juice. On the other hand, in vivo it was observed in 12 healthy male volunteers that the consumption of tropical fruit (banana) or fruit juices (orange and pineapple) increased serum melatonin concentration and the highest value was observed 120 min post intake. That is, pineapple had 146 pg/mL compared to 48 pg/mL (p = 0.002), orange had 151 pg/mL compared to 40 pg/mL. In addition, the serum antioxidant capacity also increased markedly, as shown by the significant increases in two indicators, ferric reducing antioxidant power and oxygen radical antioxidant capacity [38,45].
8. Foods containing Melatonin
The majority of food databases do not list the amount of melatonin in foods, but based on available research, mentioned six foods contain high melatonin based on a recent report in 2020. Tart cherry juice is a well-known sleep aid. Researchers have discovered that it increases melatonin levels in the body and enhances sleep. The healthier way to get melatonin is to eat cherries instead of drinking their juice. Goji berry is a fruit produced by a plant native to China. Goji berries are touted for their anti-aging properties. As well as being high in melatonin, they may contribute to improved sleep. Eggs are one of the best sources of melatonin among animal products. A warm glass of milk is a traditional remedy for insomnia, so there is no surprise it's high in melatonin. Fish is a better source of melatonin than meats. Sardines and salmon, which provide omega-3 fatty acids, are excellent choices. Also, nuts contain a good amount of melatonin. Almonds and pistachios are particularly high in melatonin [38,49].
9. Conclusion and Future recommendation
The sleep cycle of the entire population has been distorted during the COVID era. Managing coronasomnia in the COVID era may be the best way to deal with this disturbing trend. Melatonin regulates circadian rhythms and has powerful antioxidant properties and will benefit both COVID-19 patients also the COVID -19 generation. However, there is limited research of interventions using melatonin in the diet of COVID-19 generations. We have suggested that melatonin used as a supplement in tablet or injectable forms might have hidden disadvantages. Therefore, melatonin ingested as a natural dietary supplement needs consideration. Dietary supplementation may regulate the sleep cycle, and may impact on the regulation of the entire biological cycle. Although the bioavailable quantity of melatonin obtained from the diet is low, it is safer than stronger synthetically derived supplements. Future research on how we can increase the bioavailability of melatonin from food supplements is required as a matter of urgency in the treatment of coronasomnia.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
This study was supported by the Hong Kong Research Grants Council Post-doctoral Fellowship Scheme (PDFS2021-2H01).
Conflicts of interest
The authors declare no conflict of interest.
References
- BBC The “coronasomnia” phenomenon keeping you from getting sleep (2022).
- Fry A. Coronasomnia: Definition, Symptoms, and Solutions (2022).
- Gao C, Scullin MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med 73 (2020): 1-10.
- Yang M, He P, Xu X, et al. Disrupted rhythms of life, work and entertainment and their associations with psychological impacts under the stress of the COVID-19 pandemic: A survey in 5854 Chinese people with different sociodemographic backgrounds. Plos One 16 (2021): e0250770.
- Potter DM, Cade J, Grant PJ, et al. Nutrition and the circadian system. Br J Nutr 116 (2016): 434-442.
- Rondanelli M, Opizzi A, Monteferrario F, et al. The effect of Melatonin, Magnesium, and Zinc on Primary Insomnia in Long-Term Care Facility Residents in Italy: A Double-Blind, Placebo-Controlled Clinical Trial. J Am Geriatr Soc 59 (2011): 82-90.
- Zhang R, Wang X, Ni L, et al. COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250 (2020): 117583.
- Reiter R.J, Abreu-Gonzalez P, Marik PE, et al. Therapeutic algorithm for use of melatonin in patients with COVID-19. Front Med 7 (2020).
- UCSF health melatonin and sleeping pills (2022).
- NIH Melatonin: What you need to know (2021).
- Seabra M, Bignotto M, Pinto Jr, et al. Randomized, double-blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment. J Pineal Res 29 (2000): 193-200.
- Andersen LPH, Rosenberg J, Gögenur I. Perioperative melatonin: not ready for prime time. Br J Anaesth 112 (2014): 7-8.
- Jahnke G. Maternal and developmental toxicity evaluation of melatonin administered orally to pregnant Sprague-Dawley rats Toxicol Sci 50 (1999): 271-279.
- Doghramji K. Melatonin and its receptors: a new class of sleep-promoting agents. J Clin Sleep Med 3 (2007): S17-23.
- Internet the role and functions of Suprachiasmatic Nucleus (SCN) for Sleep-wake Regulation (2020).
- Agez L, Laurent V, Guerrero HY, et al F. Endogenous melatonin provides an effective circadian message to both the suprachiasmatic nuclei and the pars tuberalis of the rat. J. Pineal Res 46 (2009): 95-105.
- Lufkin B. Disrupted routines and ongoing uncertainty are contributing to a surge in insomnia. What can we do about it? (2022).
- Cleveland clinic How the COVID-19 pandemic can impact your sleep (2022).
- Morin CM, Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med 77 (2021): 346-347.
- Meaklim H, Junge MF, Varma P, et al. Pre-existing and post-pandemic insomnia symptoms are associated with high levels of stress, anxiety, and depression globally during the COVID-19 pandemic. J. Clin. Sleep Med 17 (2021): 2085-2097.
- Morin CM, Vézina-Im LA, Ivers H, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic 2020. Sleep 45 (2022).
- Zhang Y, Ren R, Lei F, et al. Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev 45 (2019): 1-17.
- How pandemic has affected homemakers (2022).
- Yoosefi Lebni J, Irandoost SF, Xosravi T, et al. Explaining the problems faced by Iranian housewives during the COVID-19 quarantine period, and their adaption strategies: A qualitative study. Women’s Heal 17 (2021).
- Guy J. Employees working from home are putting in longer hours than before the pandemic (2022).
- Sharma M, Aggarwal S, Madaan P, et al. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med 84 (2021): 259-267.
- Wang G, Zhang Y, Zhao J, et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395 (2020): 945-947.
- Cellini N, Canale N, Mioni G, et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res 29 (2020).
- Bruni O, Giallonardo M, Sacco R, et al. The impact of lockdown on sleep patterns of children and adolescents with ADHD. J. Clin. Sleep Med 17 (2021): 1759-1765.
- The Guardian Children’s sleep severely affected by impact of coronavirus, say experts (2022).
- Moon E, Partonen T, Beaulieu S, et al. Melatonergic agents influence the sleep-wake and circadian rhythms in healthy and psychiatric participants: a systematic review and meta-analysis of randomized controlled trials. Neuropsychopharmacology (2022).
- Lipman F. The truth about this popular sleep supplement- and whether it’s right for you (2022).
- Weishaupt JH, Bartels C, Pölking E, et al. Reduced oxidative damage in ALS by high-dose enteral melatonin treatment. J. Pineal Res 41 (2006): 313-323.
- Zhdanova IV, Wurtman R.J, Morabito C, et al. Effects of low oral doses of melatonin, given 2-4 hours before habitual bedtime, on sleep in normal young humans. Sleep 19 (1996): 423-431.
- Aulinas A. Physiology of the Pineal Gland and Melatonin (2000).
- Besag FMC, Vasey MJ, Lao KSJ, et al. Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: A systematic review. CNS Drugs 33 (2019): 1167-1186.
- European Food Safety Authority Scientific opinion on the substantiation of health claims related to melatonin and alleviation of subjective feelings of jet lag (ID 1953), and reduction of sleep onset latency, and improvement of sleep quality (ID 1953) pursuant to Article 13(1) of Regul. EFSA J 8 (2010).
- Meng X, Li Y, Li S, et al. Dietary sources and bioactivities of melatonin. Nutrients 9 (2017): 367.
- Zhao D, Yu Y, Shen Y, et al. Melatonin synthesis and function: Evolutionary history in animals and plants. Front. Endocrinol (Lausanne) 10 (2019).
- Musiek ES, FitzGerald GA. Molecular clocks in pharmacology (2013): 243-260.
- Kalsbeek A, Fliers E. Daily regulation of hormone profiles (2013): 185-226.
- Lully sleep insomnia meme (2022).
- Tan DX, Zanghi BM, Manchester LC, et al. Melatonin identified in meats and other food stuffs: potentially nutritional impact. J. Pineal Res 57 (2014): 213-218.
- Aguilera Y, Herrera T, Benítez V, et al. Estimation of scavenging capacity of melatonin and other antioxidants: Contribution and evaluation in germinated seeds. Food Chem 170 (2015): 203-211.
- Sae-Teaw M, Johns J, Johns NP, et al. Serum melatonin levels and antioxidant capacities after consumption of pineapple, orange, or banana by healthy male volunteers. J Pineal Res 55 (2013): 58-64.
- Oba S, Nakamura K, Sahashi Y, et al. Consumption of vegetables alters morning urinary 6-sulfatoxymelatonin concentration. J Pineal Res 45 (2008): 17-23.
- Maldonado MD, Moreno H, Calvo JR. Melatonin present in beer contributes to increase the levels of melatonin and antioxidant capacity of the human serum. Clin Nutr 28 (2009): 188-191.
- Reiter RJ, Manchester LC, Tan D. Melatonin in walnuts: Influence on levels of melatonin and total antioxidant capacity of blood. Nutrition 21 (2005): 920-924.
- WebMD Foods High in Melatonin (2022).
