Comparison of the Clinical Process Outcomes of Non-Surgical and Surgical Treatment for Cornual Pregnancy : A Retrospective Randomized Case-Control Study
Article Information
Eun Hui Joo#, Ji Hyon Jang#, Bobae Lim, Eun Hee Ahn, Sang Hee Jung, Young Ran Kim*
Department of Obstetrics and Gynecology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
*Corresponding Author: Young Ran Kim, Department of Obstetrics and Gynecology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
# - both the authors contributed equally.
Received: 20 March 2020; Accepted: 30 March 2020; Published: 03 April 2020
Citation:
Eun Hui Joo, Ji Hyon Jang, Bobae Lim, Eun Hee Ahn, Sang Hee Jung, Young Ran Kim. Comparison of the Clinical Process Outcomes of Non-Surgical and Surgical Treatment for Cornual Pregnancy : A Retrospective Randomized Case-Control Study. Journal of Women’s Health and Development 3 (2020): 065-076.
Share at FacebookAbstract
Objectives: To compare the clinical process outcomes of ultrasound (US) - guided intragestational sac injection of methotrexate (MTX) and cornual resection for cornual pregnancies.
Methods: The retrospective case-control study included 31 women diagnosed with cornual pregnancy at a single center, between January 2007 and February 2017. Of these, we enrolled 31 women who had implantation in the cornual area at the time of diagnosis; 12 were treated with local injection of MTX under ultrasound guidance and 19 underwent with cornual resection. Procedure-related outcomes, including operating time, time to normal state β-hCG serum level, and hemoglobin level changes. Statistical significance was assessed using the chi-square test, Mann-Whitney test, and Student’s t-test.
Results: Compared to the cornual resection group, the local MTX treatment group had a much shorter mean procedure time (21.64±7.18 minutes versus 60.53±5.16 minutes p< 0.01) and length of hospital stay (2.40±0.54 days versus 3.43±0.37 days, p= 0.018). Also, decreases in hemoglobin levels post-procedure were lower in the local MTX treatment group (1.59±0.16 g/dL versus 2.54±0.29 g/dL, p= 0.012). There was one case of uterine rupture in a subsequent pregnancy in the cornual resection group.
Conclusion: Non-surgical treatment has better clinical process outcomes than cornual resection for managing cornual pregnancies which desire future pregnancies without uterine rupture.
Keywords
Cornual pregnancy; Ultrasound guidance; Methotrexate; Non-surgical management
Cornual pregnancy articles Cornual pregnancy Research articles Cornual pregnancy review articles Cornual pregnancy PubMed articles Cornual pregnancy PubMed Central articles Cornual pregnancy 2023 articles Cornual pregnancy 2024 articles Cornual pregnancy Scopus articles Cornual pregnancy impact factor journals Cornual pregnancy Scopus journals Cornual pregnancy PubMed journals Cornual pregnancy medical journals Cornual pregnancy free journals Cornual pregnancy best journals Cornual pregnancy top journals Cornual pregnancy free medical journals Cornual pregnancy famous journals Cornual pregnancy Google Scholar indexed journals Ultrasound guidance articles Ultrasound guidance Research articles Ultrasound guidance review articles Ultrasound guidance PubMed articles Ultrasound guidance PubMed Central articles Ultrasound guidance 2023 articles Ultrasound guidance 2024 articles Ultrasound guidance Scopus articles Ultrasound guidance impact factor journals Ultrasound guidance Scopus journals Ultrasound guidance PubMed journals Ultrasound guidance medical journals Ultrasound guidance free journals Ultrasound guidance best journals Ultrasound guidance top journals Ultrasound guidance free medical journals Ultrasound guidance famous journals Ultrasound guidance Google Scholar indexed journals Methotrexate articles Methotrexate Research articles Methotrexate review articles Methotrexate PubMed articles Methotrexate PubMed Central articles Methotrexate 2023 articles Methotrexate 2024 articles Methotrexate Scopus articles Methotrexate impact factor journals Methotrexate Scopus journals Methotrexate PubMed journals Methotrexate medical journals Methotrexate free journals Methotrexate best journals Methotrexate top journals Methotrexate free medical journals Methotrexate famous journals Methotrexate Google Scholar indexed journals Non-surgical management articles Non-surgical management Research articles Non-surgical management review articles Non-surgical management PubMed articles Non-surgical management PubMed Central articles Non-surgical management 2023 articles Non-surgical management 2024 articles Non-surgical management Scopus articles Non-surgical management impact factor journals Non-surgical management Scopus journals Non-surgical management PubMed journals Non-surgical management medical journals Non-surgical management free journals Non-surgical management best journals Non-surgical management top journals Non-surgical management free medical journals Non-surgical management famous journals Non-surgical management Google Scholar indexed journals ectopic articles ectopic Research articles ectopic review articles ectopic PubMed articles ectopic PubMed Central articles ectopic 2023 articles ectopic 2024 articles ectopic Scopus articles ectopic impact factor journals ectopic Scopus journals ectopic PubMed journals ectopic medical journals ectopic free journals ectopic best journals ectopic top journals ectopic free medical journals ectopic famous journals ectopic Google Scholar indexed journals gonadotropin articles gonadotropin Research articles gonadotropin review articles gonadotropin PubMed articles gonadotropin PubMed Central articles gonadotropin 2023 articles gonadotropin 2024 articles gonadotropin Scopus articles gonadotropin impact factor journals gonadotropin Scopus journals gonadotropin PubMed journals gonadotropin medical journals gonadotropin free journals gonadotropin best journals gonadotropin top journals gonadotropin free medical journals gonadotropin famous journals gonadotropin Google Scholar indexed journals diagnosis articles diagnosis Research articles diagnosis review articles diagnosis PubMed articles diagnosis PubMed Central articles diagnosis 2023 articles diagnosis 2024 articles diagnosis Scopus articles diagnosis impact factor journals diagnosis Scopus journals diagnosis PubMed journals diagnosis medical journals diagnosis free journals diagnosis best journals diagnosis top journals diagnosis free medical journals diagnosis famous journals diagnosis Google Scholar indexed journals uterine artery articles uterine artery Research articles uterine artery review articles uterine artery PubMed articles uterine artery PubMed Central articles uterine artery 2023 articles uterine artery 2024 articles uterine artery Scopus articles uterine artery impact factor journals uterine artery Scopus journals uterine artery PubMed journals uterine artery medical journals uterine artery free journals uterine artery best journals uterine artery top journals uterine artery free medical journals uterine artery famous journals uterine artery Google Scholar indexed journals hemodynamically articles hemodynamically Research articles hemodynamically review articles hemodynamically PubMed articles hemodynamically PubMed Central articles hemodynamically 2023 articles hemodynamically 2024 articles hemodynamically Scopus articles hemodynamically impact factor journals hemodynamically Scopus journals hemodynamically PubMed journals hemodynamically medical journals hemodynamically free journals hemodynamically best journals hemodynamically top journals hemodynamically free medical journals hemodynamically famous journals hemodynamically Google Scholar indexed journals methotrexate articles methotrexate Research articles methotrexate review articles methotrexate PubMed articles methotrexate PubMed Central articles methotrexate 2023 articles methotrexate 2024 articles methotrexate Scopus articles methotrexate impact factor journals methotrexate Scopus journals methotrexate PubMed journals methotrexate medical journals methotrexate free journals methotrexate best journals methotrexate top journals methotrexate free medical journals methotrexate famous journals methotrexate Google Scholar indexed journals
Article Details
Introduction
Cornual pregnancy is a rare type of ectopic pregnancy where implantation occurs in the cavity of a rudimentary horn of the uterus, which may or may not be communicating with the uterine cavity. Cornual pregnancy is also described as ‘interstitial’ or ‘angular’ pregnancy in many other literatures [1], but in this article, we only use the term ‘cornual’ pregnancy. The frequency of ectopic pregnancy is 1 in 122 live births [2] and cornual pregnancies account for 2–4% of all ectopic pregnancies. It is also said to have a mortality rate in the range of 2.0-2.5% [3]. With the development of assisted reproductive technology (ART), this figure has increased to 7.3% and it may be related to a higher incidence of previous salpingectomy and tubal infertility [4]. As the previously known articles, most of all surgical management has been associated with morbidity and unfavorable sequences on fertility, more conservative approaches such as MTX local injection on cornual ectopic pregnancy area have been receiving favorable response and introduced into clinical practice recently. As women’s child-bearing age getting delayed in modern society, the improvement of ART is developing rapidly and it is possibly related to the increased rates of cornual or heterotopic pregnancies. The diagnosis of cornual pregnancy is commonly delayed because of implantation in the more vascular uterine muscular wall; therefore, sequential late management can lead to life-threatening conditions [5, 6]. Early diagnosis and treatment are important to prevent severe hemorrhagic complications. Currently, the rapid measurement of serum beta- human chorionic gonadotropin (β-hCG) levels and the improvement in ultrasonographic imaging have permitted earlier and more accurate diagnosis of cornual pregnancy, facilitating the preservation of the future fertility without causing maternal morbidity and mortality [7].
Yet, there is no academic consensus in the literature that which is the most effective treatment for cornual pregnancy. For the most part, surgical treatment has been recommended for patients with pain or hemoperitoneum [6]. However, whether surgical or non-surgical treatment should be used for asymptomatic women remains a matter of debate. Nevertheless, there is an increased risk of uterine rupture in a subsequent pregnancy following surgical treatment, possibly because of uterine scarring [8]. The overall rate of uterine rupture was reported as 3.8 per 10,000 deliveries, and this increased to 16% of all deliveries following laparoscopic wedge resection of cornual pregnancies [9].
As already mentioned, treatment of cornual pregnancy can be divided into largely two approaches, surgical or medical treatment. Surgical treatment includes laparotomy, laparoscopic procedures, and hysteroscopic procedures. On the other hand, medical treatments include systemic methotrexate, Laparoscopic guided methotrexate/potassium chloride, systemic methotrexate, and selective uterine artery embolization including of US guided local methotrexate [10]. Early diagnosis of cornual pregnancies allows the option of treatment with intragestational methotrexate (MTX) injection, which has been recognized as a safer and better method of treatment than expectant management if early diagnosis of cornual pregnancy is made hemodynamically stable condition [11]. However, there have been few reports regarding the efficacy of treatment of cornual pregnancy. Considering that there is a low incidence of cornual pregnancy, few studies have evaluated the safety of MTX local injection as well as the factors influencing the processes of the treatment [12].
Therefore, this study aimed to compare the clinical process outcomes of local MTX injection to that of cornual resection for the treatment of cornual pregnancy in a hemodynamically stable state.
Methods
We evaluated medical and ultrasonographic reports over a 10- year period using a retrospective, case-control study in the Department of Obstetrics and Gynecology of CHA Bundang Medical Center. Review of all medical records was approved by the appropriate hospital ethics committee (IRB file No CHAMC 2018-06-039-002). The records of all women who visited the hospital for treatment of cornual pregnancy between January 2007 and February 2017 were reviewed and the following data were retrieved: maternal age, parity, gestational age, previous cesarean deliveries, previous abortion, clinical presentation, ultrasonographic findings, mean gestational distance, initial serum β-hCG level, treatment method, and time to resolution to normal values of β-hCG. The ultrasonography images were reviewed by the authors according to standard ultrasonography criteria [1]. The criteria used for the diagnosis of cornual pregnancy were those proposed by Timor-Tritsch et al. to diagnose cornual pregnancies (specificity 88%–93%, sensitivity 40%): (I) an empty uterine cavity; (II) a chorionic sac separate ( > 1 cm) from the lateral edge of the uterine cavity; and (III) a thin (< 5 mm) myometrial layer surrounding the chorionic sac [13].
Over the 10- year period, a total of 236 patients were diagnosed with cornual pregnancies. Of these, we excluded 205 women, including 178 patients treated with the combined treatment method and 27 patients who underwent laparotomy because of unstable vital signs or need for transfusion. The data for the remaining 31 women diagnosed with cornual pregnancy were included in the analysis. These 31 women were divided into 2 treatment groups one group treated with local MTX injection (local MTX group, n = 12), and the other treated with cornual resection (cornual resection group, n =19).
Diagnosis and treatment
The diagnostic standard of transvaginal and three-dimensional (3D) ultrasonography (Philips, ATL 5000), and β-hCG level were applied for diagnosis as well as follow-up. There are some diagnostic difficulties in clearly elucidating the location of the gestational sac with two-dimensional (2D) ultrasonography; therefore, 3D sonography is an important imaging modality for the diagnosis of cornual pregnancy because it allows the precise location of the gestational sac, differentiating it from an eccentrically located gestational sac (Figure 1).
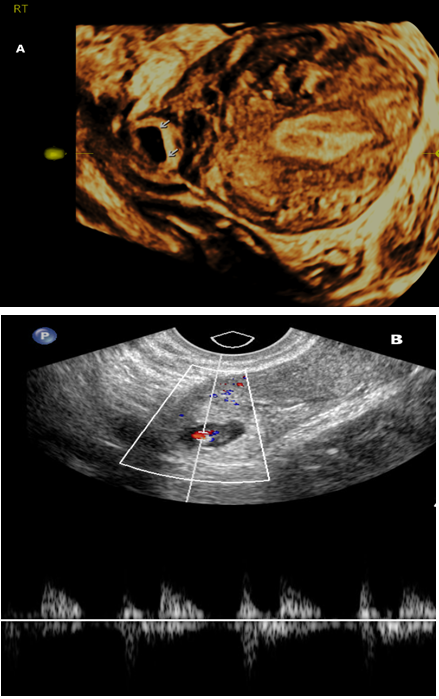
Figure 1: (a) two-dimensional (b) ultrasonography of the uterus showing gestational sac embedded in the right cornu. Uterine cavity and musculature are also seen clearly
The diagnosis using transvaginal 2D ultrasound images was based on the following criteria: (I) a vacant uterine cavity with separate gestational sac <1 cm from the most lateral edge of the uterine cavity, and a thin myometrial layer surrounding the sac; (II) a vacant cervical canal; (III) a gestational sac, with or without fetal cardiac activity, located in the upper and lateral uterine cavity of an anatomically normal uterus; (IV) an interstitial line sign corresponding to a thin echogenic line extending directly up to the center of the ectopic pregnancy; and (V) a gestational sac seen separately from the most lateral edge of the uterine cavity, with myometrium between the sac and endometrial cavity [1].
The 12 patients in the local MTX group received an injection of MTX 25 mg/mL solution (1 mg/kg, body surface area) directly into the cornual lesion. The sono-guided MTX injection procedures were performed as follow. Under no anesthesia, a 20-gauge needle was inserted into the sac using a puncture instrument (GIP; Wilson-Cook) by transvaginal ultrasonography. After aspiration of the celomic fluid, MTX was injected directly in the gestational sac (Figure 2). The procedure was performed in the operating room and no general anesthesia was used, although arrangements had been made for general anesthesia in the event of an emergency. Nevertheless, we prepared for situations where emergency exploratory surgery may be necessary ensuring abundant surrounding vessels in the cornual area of the uterus. No immediate procedure-related complications occurred. Ultrasonography was performed for approximately a few minutes after the injection to confirm that the procedure was complete without any post-procedural complications.

Figure 2: A 20-gauge needle was inserted into the sac using a puncture instrument (GIP; Wilson-Cook) by transvaginal ultrasonography and MTX was injected directly in the gestational sac.
After local administration of MTX, patients were followed up with weekly outpatient clinic visits and measurements of serum β-hCG levels. Once β-hCG levels declined to < 30 IU/L, an ultrasound examination was performed to evaluate the size of the retained products of the pregnancy. Ultrasound examinations were then performed on a monthly basis until it was confirmed that all pregnancy tissue had been spontaneously removed or absorbed.
The 19 women in the cornual resection group underwent surgery. The operation was initiated by injecting diluted vasopressin (20 U in 60-100 mL of normal saline) into the surrounding cornual myometrium. The most commonly used technique was deep circumferential incision around the cornual pregnancy implantation site at first, followed by removal of the underlying myometrium and conceptual tissue. After removal of the conceptual tissue, suturing with Vicryl l-0 was performed at the cornual resection site.
Statistical analysis
Data were analyzed using SPSS® software, version 23(IBM Corporation, Armonk, NY, USA). Continuous and ordinal data were presented as mean±standard deviation (SD), whereas categorical data were presented as absolute counts and percentages. Statistical analysis was performed using the SPSS package (SPSS, Chicago, IL, USA). Statistical significance was assessed using the chi-square test, Mann-Whitney test, and Student’s t-test. Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated. Values of p < 0.05 with confidence intervals not crossing one were used to indicate statistical significance.
Results
The clinical characteristics of the pregnancies are shown in Table 1. A total of 31 patients who were hemodynamically stable and had unruptured cornual pregnancies were enrolled. There were no statistically significant differences between the groups with respect to maternal age, gravidity, previous caesarean deliveries, previous dilatation and evacuation or previous history of gynecologic surgery. However, the cornual resection group had significantly higher parity (1.00±0.38 versus 0.30±0.15, p=0.020).
|
Characteristics |
Cornual pregnancies (n=31) |
Local injection(n=12) |
Cornual resection (n=19) |
P value |
|
Age(years) |
32.94±1.11 |
32.20±0.94 |
34.00±2.40 |
0.535 † |
|
BMI (kg/m2) |
21.66±0.45 |
21.54±0.90 |
21.74±0.50 |
0.589 † |
|
Gravidity |
1.59±0.33 |
1.20±0.25 |
2.14±0.70 |
0.059 † |
|
Parity |
0.59±0.19 |
0.30±0.15 |
1.00±0.38 |
0.020* |
|
History of D&C |
1.09±0.12 |
1.00±0.20 |
1.11±0.15 |
0.958 † |
|
History of C/S |
0.27±0.95 |
0.09±0.09 |
0.37±0.10 |
0.132 † |
|
History of D&C or Hysteroscopy |
4(12.9%) |
2(16.7%) |
2(10.5%) |
0.630 ‡ |
|
History of surgery involving uterus |
2(6.5%) |
1(8.3%) |
1(5.3%) |
1.000 ‡ |
|
History of surgery involving adnexa |
6(19.4%) |
4(33.3%) |
2(10.5%) |
0.174 ‡ |
|
No previous pelvic surgery |
13(41.9%) |
4(33.3%) |
9(47.45) |
0.440 ‡ |
D&C: dilatation and curettage, C/S: cesarean section, BMI: body mass index
Data are expressed as mean±SD or number (%)
*Data are analyzed with Student’s t-test
† Data are analyzed with Mann-Whitney test
‡ Data are analyzed with Chi-squared test
Table 1: Demographic data of the two subgroups according to treatment method
The mean age was 32.94±1.11 years and the mean number of abortions was 1.09±0.12. The mean serum β-hCG level at the time of initial diagnosis was 23322.18±5776.71 mIU/mL and the mean gestational age was 6.50±0.51 weeks.
Local MTX injection treatment is a relatively new method for removing conceptual tissue without disturbing the normal myometrium of the uterus; it offers several benefits in that it does not require general anesthesia.
Serial β-hCG measurements and clinical outcomes were compared between the groups. The mean initial β-hCG level at the time of diagnosis was 26411.60±9719.63 mIU/mL in the local MTX treatment group, and 18908.71±2855.75 mIU/mL in the cornual resection group (p = 0.605, Table 2). The results of the two groups according to treatment method are represented in Table 3. Compared with the cornual resection group, the local MTX treatment group had a shorter length of hospital stay (2.40±0.54 versus 3.43±0.37, p=0.018), and a smaller decrease in the hemoglobin level after the procedure (1.59±0.16 versus 2.54±0.29, p=0.012). The mean operation times were 21.64±7.18 minutes in the local injection group and 60.53 ± 5.16 minutes in the cornual resection group (p <0.01).
|
Characteristics |
Cornual pregnancies(n=31) |
Local injection(n=12) |
Cornual resection(n=19) |
P value |
|
Gestational age(wk.) |
6.50±0.51 |
6.70±0.49 |
6.22±1.06 |
0.675* |
|
β-hCG (mIU/mL) |
23322.18±5776.71 |
26411.60±9719.63 |
18908.71±2855.75 |
0.605* |
|
Conception mode – spontaneous |
29(93.5%) |
11(91.7%) |
18(94.7%) |
1.000 ‡ |
|
Conception mode – IVF |
2(6.5%) |
1(8.3%) |
1(5.3%) |
1.000 ‡ |
|
MGD (mm) |
15.17±1.60 |
16.04±2.56 |
13.93±1.46 |
0.578* |
|
CRL (mm) |
5.72±0.93 |
5.98±1.58 |
5.36±0.45 |
0.336* |
|
Cornual mass mean diameter (mm) |
27.74±1.84 |
27.50±2.99 |
28.09±1.65 |
0.448* |
|
Clinical symptom – abdominal pain |
9(29.0%) |
1(8.3%) |
8(42.1%) |
0.101 ‡ |
|
Clinical symptom – vaginal spotting |
1(3.2%) |
0(0%) |
1(5.3%) |
1.000 ‡ |
|
No clinical symptom |
22(71.0%) |
11(91.7%) |
11(57.9%) |
0.044 ‡ |
β-hCG: beta human chorionic gonadotropin, IVF: in vitro fertilization, MGD: Mean gestational sac diameter, CRL: crown-rump length
Data are expressed as mean±SD or number (%)
*Data are analyzed with Student’s t-test
2Data are analyzed with Mann-Whitney test
‡ Data are analyzed with Chi-squared test
Table 2: Presentation of the 2 subgroups according to treatment method at diagnosis
|
Characteristics |
Cornual pregnancies (n=31) |
Local injection (n=12) |
Cornual resection (n=19) |
P value |
|
Length of hospital stay (day) |
2.82±0.37 |
2.40±0.54 |
3.43±0.37 |
0.018 † |
|
Extent of Hb level decrease (g/dL) |
1.98±0.19 |
1.59±0.16 |
2.54±0.29 |
0.012 † |
|
Time to normal β-hCG (day) |
41.51±11.14 |
68.90±13.13 |
2.37±0.45 |
<0.01* |
|
Duration of follow up after treatment (day) |
39.76±7.18 |
50.30±9.52 |
24.71±8.71 |
0.008 † |
|
Treatment failure |
1(3.2%) |
1(8.3%) |
0(0%) |
0.387 ‡ |
|
Subsequent pregnancy outcome |
7(22.6%) |
3(25.0%) |
4(21.1%) |
1.000 ‡ |
|
Operation time (min) |
46.27±5.39 |
21.64±7.18 |
60.53±5.16 |
<0.01 † |
Hb: Hemoglobin
Data are expressed as mean±SD or number (%)
*Data are analyzed with Student’s t-test
† Data are analyzed with Mann-Whitney test
‡ Data are analyzed with Chi-squared test
Table 3: Results of the 2 subgroups according to treatment method
Fertility follow-up was performed up to 24 months post-procedure. The subsequent pregnancy outcomes showed no significant differences because of the small number of samples; nevertheless, there was one patient with cornual rupture in a subsequent pregnancy in the cornual resection group.
There were no side-effects following local MTX treatment, and no severe adverse effects such as leukopenia, thrombocytopenia, liver toxicity, or hair loss were noted.
Discussion
Of the 12 women who were treated with local MTX injection, 11 were treated successfully. There are various medical (non-surgical) and surgical treatment approaches for cornual pregnancy. The treatments traditionally described for cornual pregnancy are laparotomy, cornual resection, and hysterectomy. However, these are associated with a high possibility of uterine rupture during subsequent pregnancies, as well as detrimental effects on future fertility
Most women with cornual pregnancy are of reproductive age and desire future fertility. The ideal treatment regime should be designed to eliminate the cornual pregnancy without damage to the uterine myometrium and alternatives exist in this regard including expectant management, systemic MTX administration, local MTX injection, or a combination of both expectant management and local MTX injection [5].
Medical or minimally invasive treatments are preferable to surgical interventions. Several medical treatments, including local MTX and potassium chloride injection, have been introduced with generally satisfactory results [14]. Despite the fact that medical treatment has been used successfully, the duration of treatment is long, and the risk of rupture persists during therapy [15]. In the present study, we noted a longer mean duration of follow-up after treatment with local MTX injection than with cornual resection. There were no subsequent uterine ruptures in women treated with local MTX. By contrast, one patient in the cornual resection group experienced uterine rupture during a subsequent pregnancy [16]. A risk factor for uterine rupture in subsequent pregnancies is previous pelvic surgery involving the uterus [9]. In our series, one woman who had undergone a laparoscopic left cornual resection two years previously was found to have a thin uterine wall with a fetal part beneath it on ultrasound examination at 33 weeks and 3 days of gestation (Figure 3), suggesting a uterine rupture. Emergency exploratory laparotomy was performed and a 2,604 g male baby was delivered with Apgar scores of 6 at 1and 8 at 5 minutes.

Figure 3: Uterine wall defect and extruded amniotic sac with the fetal buttocks in the uterine rupture. AF: amniotic fluid; M: myometrium; P: placenta
Currently, laparoscopic surgery is widely used to treat cornual pregnancy with embryo heart beat activity or symptomatic signs. However, as shown in our study, the disadvantages of cornual resection over MTX injection are that the length of hospital stay is longer, the decrease in hemoglobin level before and after the procedure is greater, and the procedure time is significantly longer. Furthermore, one of the main problems in this situation, particularly after wedge resection, is uterine rupture in a subsequent pregnancy. Therefore, local MTX treatment provided results equivalent to those of surgical treatment, with the advantage of maintaining fertility without the risk of uterine rupture.
It is believed that local MTX injection may be used to successfully to treat a cornual pregnancy rather than other ectopic pregnancies because the surrounding deep myometrium permits more expansion than does the tube, allowing sealing off of the uterine circulation and accumulation of MTX inside the intragestational sac. Local intragestational MTX injection is therefore a useful treatment option for cornual pregnancy because of the prompt response and lack of adverse effects. Moreover, advances in imaging sonography (2D or 3D) technology enable earlier diagnosis before the onset of an unstable state, when non-surgical management can be feasible access as a treatment of choice. The sono-guided injection of MTX has advantages over surgical treatment because it is less invasive and inexpensive, with less operative morbidity and minimal blood loss. Bnifla et al. demonstrated three cases of heterotopic cornual pregnancy successfully treated with local injection [17]. It may also be a treatment option for heterotopic pregnancies, that are increasing in number since the development of ART, although this has not yet been formally established. Local MTX injection may be better than systemic MTX treatment for cornual pregnancies that are part of a heterotopic pregnancy, in view of the adverse effects of MTX on intrauterine pregnancy.
There were some limitations to this study. This was a retrospective case control study with a small number of patients with cornual pregnancy. A large study sample should be enrolled in future studies to obtain more meaningful results, including those regarding maternal morbidity and subsequent fertility. Furthermore, it is necessary to carry out large prospective randomized trials. Such a study would further validate the safety of local MTX injection in the preservation of the uterus without damage to the myometrium.
There are several strengths of this study. It is the first study to directly compare the clinical process outcomes of local MTX treatment and cornual resection in terms of the hemodynamic state. Second, the local MTX treatment group included patients with older gestational age, larger mean gestational sac diameter size, and higher initial β-hCG levels. Moreover, the data were not influenced by procedure related variability, because local MTX injection was performed by a single physician, and the surgery was performed by two highly skilled physicians.
In conclusion, the treatment outcome after local MTX treatment was comparable to that after cornual resection, and local MTX treatment significantly reduced the procedure time and extent of hemoglobin level decrease. In addition, this method offers benefit of no requirement of general anesthesia. Fertility and obstetric outcomes following cornual pregnancy are affected show a significant difference according to initial treatment. As shown in our results, local MTX treatment showed better clinical process outcomes than did cornual resection as a first-line treatment option. In this regard, if early diagnosis of cornual pregnancy is made, this procedure can be considered first, especially for women with heterotopic pregnancies in hemodynamically stable states who desire to become pregnant in the future.
Acknowledgments
This research were supported by the CHAbiotec: grant number 2017061665 and the study of The Establishment and Characteriazation of placneta-derived Stm cell Band for Cell therapy (IRB File No.2019-10-035)
Conflicts of interest
The authors declare that they have no competing interests.
References
- Arleo EK, DeFilippis EM. Cornual, interstitial, and angular pregnancies: clarifying the terms and a review of the literature. Clinical Imaging 38 (2014): 763-770.
- Escobar-Padilla B, Perez-Lopez CA, Martinez-Puon H. Risk factors and clinical features of ectopic pregnancy. Revista Medica del Instituto Mexicano del Seguro Social 55 (2017): 278-285.
- Faraj R, Steel M. Management of cornual (interstitial) pregnancy. The Obstetrician & Gynaecologist 9 (2007): 249-255.
- Wang J, Huang D, Lin X, Saravelos SH, Chen J, Zhang X, Li T, Zhang S. Incidence of Interstitial Pregnancy After In Vitro Fertilization/Embryo Transfer and the Outcome of a Consecutive Series of 38 Cases Managed by Laparoscopic Cornuostomy or Cornual Repair. Journal of Minimally Invasive Gynecology 23 (2016): 739-747.
- Lau S, Tulandi T. Conservative medical and surgical management of interstitial ectopic pregnancy. Fertility and Sterility 72 (1999): 207-215.
- Hoyos LR, Vilchez G, Allsworth JE, Malik M, Rodriguez-Kovacs J, Adekola H, Awonuga AO. Outcomes in subsequent pregnancies after wedge resection for interstitial ectopic pregnancy: a retrospective cohort study. Journal of Maternal-Fetal & Neonatal Medicine 32 (2019): 2354-2360.
- Litwicka K, Greco E, Prefumo F, Fratelli N, Scarselli F, Ferrero S, Iammarrone E, Frusca T. Successful management of a triplet heterotopic caesarean scar pregnancy after in vitro fertilization-embryo transfer. Fertility and Sterility 95 (2011): 291.e291-293.
- Arbab F, Boulieu D, Bied V, Payan F, Lornage J, Guerin JF. Uterine rupture in first or second trimester of pregnancy after in-vitro fertilization and embryo transfer. Human Reproduction 11 (1996): 1120-1122.
- Chao AS, Chang YL, Yang LY, Chao A, Chang WY, Su SY, Wang CJ. Laparoscopic uterine surgery as a risk factor for uterine rupture during pregnancy. PloS One 13 (2018): e0197307.
- Chu AY, Deng X, Fisher VA, Drong A, Zhang Y, Feitosa MF, Liu C-T, Weeks O, Choh AC, Duan Q. Multiethnic genome-wide meta-analysis of ectopic fat depots identifies loci associated with adipocyte development and differentiation. Nature Genetics 49 (2017): 125-130.
- Kim YR, Moon MJ. Ultrasound-guided local injection of methotrexate and systemic intramuscular methotrexate in the treatment of cesarean scar pregnancy. Obstetrics & Gynecology Science 61 (2018): 147-153.
- Prenaud C, Scherier S, Malgras B. Management of a cornual ectopic pregnancy. Journal of Visceral Surgery 154 (2017): 467-468.
- Timor-Tritsch IE, Monteagudo A, Matera C, Veit CR. Sonographic evolution of cornual pregnancies treated without surgery. Obstetrics and Gynecology 79 (1992): 1044-1049.
- Sagiv R, Debby A, Keidar R, Kerner R, Golan A. Interstitial pregnancy management and subsequent pregnancy outcome. Acta Obstetricia et Gynecologica Scandinavica 92 (2013): 1327-1330.
- Lee MH, Im SY, Kim MK, Shin SY, Park WI. Comparison of Laparoscopic Cornual Resection and Cornuotomy for Interstitial Pregnancy. Journal of Minimally Invasive Gynecology 24 (2017): 397-401.
- Lee GM, Jang HY, Chang SW, Jong SH, Moon MJ, Kim YR, Ahn EH. Recurrent spontaneous uterine rupture during the third trimester in a woman with history of laparoscopic cornual resection and cervical dysplasia. Korean Journal of Obstetrics and Gynecology 55 (2012): 973-977.
- Benifla JL, Fernandez H, Sebban E, Darai E, Frydman R, Madelenat P. Alternative to surgery of treatment of unruptured interstitial pregnancy: 15 cases of medical treatment. European Journal of Obstetrics, Gynecology, and Reproductive Biology 70 (1996): 151-156.
