Comparison of Diabetogenic and Lipid Profile Among Vitamin D Deficient and Non-deficient Male Subjects
Article Information
Sikandar Hayat Khan1*, Abdul Rahim Khan2, Rahat Shahid3, Robina Manzoor4
1Department of pathology PNS HAFEEZ, Pakistan
2Bedford Hospital NHS Trust Hospital, UK
3Department of Radiology PNS HAFEEZ Hospital, Pakistan
4Department of gynecology PNS HAFEEZ, Pakistan
*Corresponding author: Dr. Sikandar Hayat Khan, Department of pathology PNS HAFEEZ, Pakistan
Received: 07 November 2020; Accepted: 16 November 2020; Published: 27 November 2020
Citation: Sikandar Hayat Khan, Abdul Rahim Khan, Rahat Shahid, Robina Manzoor. Comparison of Diabetogenic and Lipid Profile Among Vitamin D Deficient and Non-deficient Male Subjects. Archives of Clinical and Biomedical Research 4 (2020): 728-737.
Share at FacebookAbstract
Objective: To evaluate diabetogenic and lipid profiles among subjects with or without vitamin D deficient male subjects.
Design: Cross-sectional analysis Place and duration of study: From Jan- 2018 to Dec- 2018 at PNS HAFEEZ hospital Islamabad
Subjects and methods: From a target population of adult male patients selected after several exclusion, we had a final total sample size of 133, which were evaluated among two groups formulated based upon whether having vitamin D deficiency or otherwise. We further compared diabetic and lipid indices including fasting plasma glucose, glycated hemoglobin (HbA1c), total cholesterol, fasting triglycerides, LDL cholesterol and HDL cholesterol among the vitamin D deficient group and vitamin D non-deficient groups by using Independent sample t-statistics.
Results: HbA1c levels were higher in subjects with vitamin D deficiency [Mean: 7.43% (+2.45), n=87] in comparison to non-vitamin D deficient subjects [Mean: 6.54% (+1.67), n=45], (p=0.029). Fasting plasma glucose levels were higher in subjects with vitamin D deficiency [Mean: 8.12 mmol/L (+4.05), n=86] in comparison to non-vitamin D deficient subjects [Mean: 6.88 mmol/L (+2.85), n=43], (p=0.074). Lipid parameters did not demonstrate statistical significance among subjects with or without vitamin D deficiency.
Conclusion: HbA1c and fasting plasma glucose levels were higher among subjects with vitamin D deficiency in comparison to non-vitamin D deficient male subjects.
Keywords
Vitamin D; Type-2 diabetes Mellitus (T2DM); HbA1c, total cholesterol; LDL-cholesterol; HDL-cholesterol and fasting triglycerides
Vitamin D articles; Type-2 diabetes Mellitus (T2DM) articles; HbA1c articles, total cholesterol articles; LDL-cholesterol articles; HDL-cholesterol and fasting triglycerides articles
Article Details
1. Introduction
Recent evidence have highlighted a link between diabetes mellitus and vitamin D deficiency, which has promoted researchers to explore vitamin D as a treatment prospects for diabetes mellitus, especially type-2 diabetes mellitus [1]. Though the functional role of vitamin D as immune modulatory agent and anti-proliferative agents are not well-documented but still the association between the two under evaluation categories is yet debatable [2]. The data with reference to vitamin D is so much prevalent on pubmed and other search engines that vitamin D seems like a panacea for multiple diseases beyond mineral or bone metabolism [3-5]. This approach has not only resulted in overambitious use of both vitamin D diagnostics, which are expensive but also exuberant use of vitamin D with most drug prescription without realization of the effects of hypervitaminosis D [6-8].
Diabetes mellitus is one such metabolic disorder which have been associated with deficient vitamin D associated in multiple studies [9,10]. Alongside there is also contrasting evidence which does not conclude an association or beneficial effect of vitamin D supplementation for diabetes mellitus [11,12]. More importantly, it seems pertinent here to quote the viewpoints of Institute of medicine (IOM) and the Endocrine Society which not only differ on the reference ranges for vitamin D, but also the former group suggest otherwise to vitamin D as potential factor for causation of type-2 diabetes mellitus [13,14]. Contrary to IOM’s stand point the Endocrine Society suggests the evidence from various observational studies to be enough for suggesting vitamin D as a as treatment modifier in type-2 diabetes mellitus [14].
Moreover, the major source of vitamin D is ultraviolet rays from sunlight, which are dispersed differentially across the globe depending upon you live in tropics or away from the equator. Similarly, the major initiator step in vitamin D metabolism is the skin where different races tolerate and utilized vitamin D different for obvious physiological and morphological differences [15]. Regional data suggests varying results as people have differential exposure to sunlight; however few studies have shown vitamin D deficiency with diabetes [16].
Questions raised include whether there is an association between vitamin D deficiency and diabetes or otherwise. Similarly, is age being a more prominent factor in causation of vitamin D deficiency than diabetes itself. The data with respect to association between diabetes and vitamin D is highly variable in literature review and it’s important to understand the link between the two categories as if vitamin D is actually deficient in diabetes, should it not be part of any anti-diabetic treatment regimen?. Therefore a study has been planned to evaluate the association of diabetes mellitus and vitamin D deficiency.
2. Methodology
This study was carried out at the department of pathology PNS HAFEEZ hospital, Islamabad after formal permission from hospital’s “ethical review committee” approval from Jan-2018 to Nov-2018 among male subjects. The sampling technique was based upon “non-probability convenience based method”. Male diabetic patients who had who of age greater than 30 years without associated ischemic heart disease or any other acute or co-morbid medical or surgical condition taking any other medicine other than anti-diabetic medication, were included in the study. Alongside age-matched male patients without any history of medical or surgical disease visiting hospital as part of executive clinical and laboratory screening were also recruited in the study. Bothe categories of patients were explained about the nature of the study, type of testing and consequent study data utilization following a written signature with a mandatory requirement for formal participation into the study. Subjects who did not further volunteer, were not in exact medical fasting status, were taking other medications including pain killers or vitamin supplements or suffering from any chronic or acute health conditions were excluded form study. After formal consent all subjects regardless of patients or controls were interviewed according to a formatted pattern, anthropometric parameters were measured as per WHO criteria. Blood was collected in Sodium fluoride, EDTA, plain gel tubes for measurement of biochemical parameters and vitamin D. Analysis of glucose and other biochemical parameters were carried out on random access clinical chemistry analyzer (Selectra proM) and vitamin D and HbA1c was analyzed by Chemi-luminescent Microparticle Immunoassay (CMIA) on ARCHITECT I system supplied by Abbot diagnostics. Glucose was measured using GOD-PAP method, while cholesterol and triglycerides were analyzed by CHOD-PAP and GPO-PAP method on Selectra-ProM clinical chemistry analyzer. LDL-cholesterol and HDL-cholesterol were measured by direct enzymatic, selective end-point method using selective detergent and direct enzymatic, selective end-point method using accelerator selective detergent method on Selectra-proM clinical chemistry analyzer.
Subjects were segregated between two groups based upon their vitamin D results: Group-1: Vitamin D deficient subjects < 30nmol/L, Group-2: Non-Vitamin D deficient subjects >30 nmol/L. Final sample count was 135 but we lost few patients (n=2 for vitamin D sample) due to technical need of sample repetition and patients didn’t turn up for follow up.
Data analysis
All data was entered into SPSS- program. Descriptive statistics for age, time spent during outdoor exercise and major dietary choice were evaluated by SPSS>analyze>descriptive statistics. Independent sample t-test was employed to measure the differences for various anthropometric, diabetogenic and lipid parameters among vitamin D deficient and non-vitamin D deficient subjects. A p-value of 0.05 was considered as significant.
3. Results
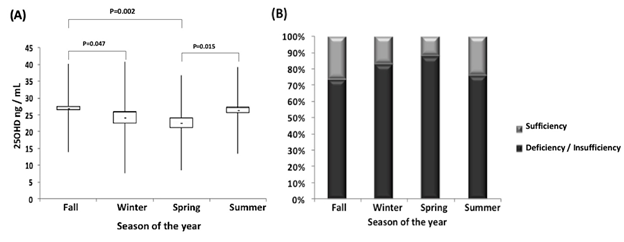
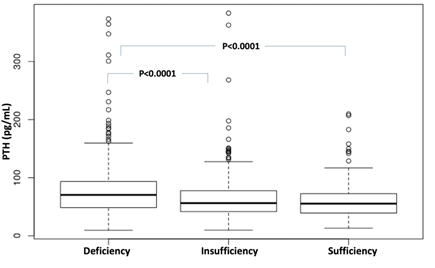
Mean age among our data subjects was 49.13 (+ 6.89) years. Most feel claim eating food from home (83%), 8.8% preferred non-homemade food, 5.2% ate both type of food whether homemade or outside and with no reply coming from 3%. In terms of exercise in outdoors. 54 subjects reported an exercise time of greater than 30 minutes in outdoors while 74 reported less than 30minutes exercise in outdoors. There was no differences between age, anthropometric indices and blood pressures between subjects having deficient vitamin D levels and non-vitamin D deficient levels as shown in Table-1 except for WHtR where it was nearly reaching statistical significance (p=0.078). HbA1c was higher in subjects with vitamin D deficiency [Mean: 7.43% (+2.45), n=87] in comparison to non-vitamin D deficient subjects [Mean: 6.54% (+1.67), n=45], (p=0.029) as shown in Figure-1. Fasting plasma glucose levels were higher in subjects with vitamin D deficiency [Mean: 8.12 mmol/L (+4.05), n=86] in comparison to non-vitamin D deficient subjects [Mean: 6.88 mmol/L (+2.85), n=43], (p=0.074) as depicted in Figure-2. Lipid parameters did not demonstrate statistical significance among subjects with or without vitamin D deficiency Table-4).
|
Parameter |
Vitamin-D based groups |
N |
Mean |
Std. Dev |
Sig. (2-tailed) |
|
Age (years) |
Vitamin D deficient subjects |
28 |
48.39 |
6.01 |
0.411 |
|
Non-vitamin D deficient subjects |
104 |
49.58 |
6.92 |
||
|
Weight (kg) |
Vitamin D deficient subjects |
28 |
82.04 |
11.71 |
0.313 |
|
Non-vitamin D deficient subjects |
105 |
79.46 |
12.03 |
||
|
Body Mass Index (kg/m2) |
Vitamin D deficient subjects |
28 |
28.63 |
4.81 |
0.261 |
|
Non-vitamin D deficient subjects |
105 |
27.38 |
5.27 |
||
|
Waist circumference (cm) |
Vitamin D deficient subjects |
28 |
97.79 |
7.96 |
0.100 |
|
Non-vitamin D deficient subjects |
105 |
94.17 |
10.78 |
||
|
Waist to height ratio (WHtR) |
Vitamin D deficient subjects |
28 |
0.58 |
0.06 |
0.078 |
|
Non-vitamin D deficient subjects |
105 |
0.55 |
0.07 |
||
|
Waist to hip ratio (WHpR) |
Vitamin D deficient subjects |
28 |
0.95 |
0.03 |
0.962 |
|
Non-vitamin D deficient subjects |
105 |
0.95 |
0.05 |
||
|
Systolic blood pressure (mm of Hg) |
Vitamin D deficient subjects |
27 |
123 |
10.68 |
0.651 |
|
Non-vitamin D deficient subjects |
104 |
121 |
16.41 |
||
|
Diastolic blood pressure (mm of Hg) |
Vitamin D deficient subjects |
27 |
83 |
8.23 |
0.301 |
|
Non-vitamin D deficient subjects |
104 |
81 |
9.09 |
Table 1: Data comparison for age, blood pressure and anthropometric profiles between vitamin D deficient and non-vitamin D deficient subjects
|
Parameter |
Vitamin D based groups |
N |
Mean |
Std. Dev |
Sig (2-tailed) |
|
Total cholesterol (mmol/L) |
Vitamin D deficient subjects |
87 |
4.62 |
1.00 |
0.832 |
|
Non-vitamin D deficient subjects |
45 |
4.66 |
1.19 |
||
|
Fasting triglycerides (mmol/L) |
Vitamin D deficient subjects |
87 |
2.03 |
1.23 |
0.676 |
|
Non-vitamin D deficient subjects |
45 |
1.93 |
1.47 |
||
|
LDL-cholesterol (mmol/L) |
Vitamin D deficient subjects |
88 |
2.49 |
0.73 |
0.798 |
|
Non-vitamin D deficient subjects |
45 |
2.53 |
0.93 |
||
|
HDL-cholesterol (mmol/L) |
Vitamin D deficient subjects |
88 |
0.89 |
0.20 |
0.802 |
|
Non-vitamin D deficient subjects |
45 |
0.89 |
0.19 |
Table 2: Differences between various lipid indices among vitamin D based groups
4. Discussion
This study has demonstrated that vitamin D deficiency is associated with diabetogenic tendencies. This patterns was clearly demonstrated for glycated hemoglobin where a clear rise in levels was observed among with vitamin D deficiency. Similarly, fasting plasma glucose results also showed lower values for subjects with higher vitamin D to ones with either insufficient or deficient vitamin D levels. Review of literature linking diabetes and vitamin D deficiency shows mixed data where both for and against notions our findings can be found. Our results, however are in accordance with most available research data [9,10,13,17]. Though supporting data, including ours is available to show a link between vitamin D and diabetes, still multiple studies are available in literature where no association was observed [11,12,14,18]. Jorde et al demonstrated in placebo controlled trial that cholecalciferol administration did not prevent type-2 diabetes mellitus even 40000 IU/week for 6 months [19]. Another recent randomized control trial by Gulseth HL et al utilizing 2000000 IU of Vitamin D3 in 62 subjects also were not able to show any improvement in insulin sensitivity or diabetes markers [20]. Pilz et al have reviewed the data on supplementing type-2 diabetic subjects with vitamin D but found them not being useful [21]. The evidence favoring our findings can be presented as: The data from experimental animal models implicate an impaired insulin secretory response in diabetes which was rapidly corrected on vitamin D supplementation [22]. Another important and pivotal finding which support our results could be the discovery of vitamin D receptors (VDR) in extra-renal tissues including pancreatic beta cells, which can signify the role of vitamin D in progression of beta cells downhill course leading towards diabetes [23]. Another physiologically important process linked to insulin secretions is the flux of calcium from beta cells which indirectly helps beta cell integrity of function [24]. Another factor linked to calcium metabolism is the cytosolic protein calbindin which apart from its calcium homeostasis maintenance in cytosol have also been associated with synthesis of insulin beta cells [25]. Moreover, other factors like the renin-angiotensin aldosterone system (RAAS) have also been demonstrated to have been affected indirectly by vitamin D to reduce insulin resistance [26]. Finally, evidence is also there about vitamin D protecting the beta cell from cytokine caused apoptosis, thus helping optimal beta cell life in time of high inflammatory presence of the TNF-alpha and NF-kB [27]. Thus the aforementioned shared physiology and supporting studies referenced above emphasize further the importance of our results [9,10,13,17,22-27].
We did not demonstrate statistically significant difference in various lipid parameters and vitamin D based groups but still worse lipid levels were observed for total cholesterol, LDL-cholesterol and triglycerides. In this regard some data in literature review may not augment our findings as highlighted by Jiang et al and Wang et al [28, 29]. Nonetheless there data supportive to our findings as highlighted by Ponda et al where lipid parameters were not improved even after vitamin D supplementation [30].
We feel certain to our study needs to be acknowledged: Firstly, we believe our study had small sample size due resource availability, hospital setting, cross-sectional design and lack of funding, so possibility of type-2 statistical error remains a possibility for lipid studies. Furthermore, we anticipate regional differences to be very pertinent as distance from equator may affect vitamin D levels uptake by skin differing between races [31]. Moreover, we also feel that a regional and race wise reference values are needed by planning an epidemiological study.
We believe our original data has got significant implications as we were able to establish an association between low vitamin D levels and indices of diabetes. Further RCTs and data may be planned therefore, to assess if pharmacological addition of vitamin D to diabetes treatment may reduce diabetes incidence and severity in known diabetic patients.
5. Conclusion
Diabetes parameter including fasting plasma glucose and HbA1c were found to be raised in vitamin D deficiency in comparison to non-vitamin D deficient male subjects. Lipid parameters did not demonstrate statistical significance among subjects with or without vitamin D deficiency.
Abbreviations: HbA1c: Glycated hemoglobin, T2DM: Type-2 diabetes mellitus, qCRP: Quantitative C-Reactive protein, UACR: Urine Albumin Creatinine Ratio, WHtR: Waist to height ratio, WHpR: Waist to hip ratio.
Ethical approval: The project “Comparison of diabetogenic and lipid profile among vitamin D deficient and non-deficient male subjects: A study from Islamabad” was approved by PNS HAFEEZ hospital’s ethical review committee. All subjects signed informed consent written consent Performa after they were explained regarding study project.
Availability of data and materials: SPSS data outputs are available for review from corresponding author, if requested.
Author’s contributions: SHK: (Corresponding author) Idea, sampling, lab testing, statistical data analysis, medical writing, discussion and conclusion, ARK: History, sampling, writing, discussion and conclusion, RS: Sampling, statistical and data analysis, RM: Data analysis, medical writing. All authors approved the final manuscript.
Consent for publication: Sign written consent was taken from all study participants.
Competing interests: The authors have declare any competing interests.
Data funding: The study had no funding source to disclose.
Acknowledgements:
The authors acknowledge the work of Mr. Amin, Lab technician Ibrahim for the support and help.
References
- Baz-Hecht M, Goldfine AB. The impact of vitamin D deficiency on diabetes and cardiovascular risk. Current Opinion in Endocrinology, Diabetes and Obesity 17 (2010): 113-119.
- Selvaraj P, Harishankar M, Afsal K. Vitamin D: Immuno-modulation and tuberculosis treatment. Canadian Journal of Physiology and Pharmacology 93 (2015): 377-384.
- Zeljic K, Supic G, Magic Z. New insights into vitamin D anticancer properties: focus on miRNA modulation. Molecular Genetics and Genomics 292 (2017): 511-524.
- Paik S, Kim JK, Chung C, et al. Autophagy: A new strategy for host-directed therapy of tuberculosis. Virulence 10 (2019): 448-459.
- Bizzaro G, Antico A, Fortunato A, et al. Vitamin D and autoimmune diseases: is vitamin D receptor (VDR) polymorphism the culprit. Isr Med Assoc J 19 (2017): 438-443.
- Health Quality Ontario. Clinical utility of vitamin d testing: an evidence-based analysis. Ont Health Technol Assess Ser 10 (2010): 1-93.
- Marcinowska-Suchowierska E, Kupisz-Urbanska M, Lukaszkiewicz J, et al. Vitamin D toxicity–a clinical perspective. Frontiers in Endocrinology 9 (2018): 550.
- Ketha H, Wadams H, Lteif A, Singh RJ. Iatrogenic vitamin D toxicity in an infant–a case report and review of literature. The Journal of Steroid Biochemistry and Molecular Biology 148 (2015): 14-18.
- Mirhosseini N, Vatanparast H, Mazidi M, et al. The effect of improved serum 25-hydroxyvitamin D status on glycemic control in diabetic patients: a meta-analysis. The Journal of Clinical Endocrinology & Metabolism 102 (2017): 3097-3110.
- Abdelsadek SE, El Saghier EO, Raheem SI. Serum 25 (OH) vitamin D level and its relation to diabetic peripheral neuropathy in Egyptian patients with type 2 diabetes mellitus. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery 54 (2018): 36.
- Lips P, Eekhoff M, van Schoor N, et al. Vitamin D and type 2 diabetes. The Journal of Steroid Biochemistry and Molecular Biology 173 (2017): 280-285.
- Moreira-Lucas TS, Duncan AM, Rabasa-Lhoret R, et al. Effect of vitamin D supplementation on oral glucose tolerance in individuals with low vitamin D status and increased risk for developing type 2 diabetes (EVIDENCE): A double-blind, randomized, placebo-controlled clinical trial. Diabetes, Obesity and Metabolism 19 (2017): 133-141.
- Rosen CJ, Abrams SA, Aloia JF, et al. IOM committee members respond to Endocrine Society vitamin D guideline. The Journal of Clinical Endocrinology & Metabolism 97 (2012): 1146-1152.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism 96 (2011): 1911-1930.
- Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 27 (2004): 2813-2818.
- Lu L, Yu Z, Pan A, et al. Plasma 25-hydroxyvitamin D concentration and metabolic syndrome among middle-aged and elderly Chinese individuals. Diabetes Care 32 (2009): 1278-1283.
- Forouhi NG, Ye Z, Rickard AP, et al. Circulating 25-hydroxyvitamin D concentration and the risk of type 2 diabetes: results from the European Prospective Investigation into Cancer (EPIC)-Norfolk cohort and updated meta-analysis of prospective studies. Diabetologia 55 (2012): 2173-2182.
- Sollid ST, Hutchinson MY, Fuskevåg OM, et al. No effect of high-dose vitamin D supplementation on glycemic status or cardiovascular risk factors in subjects with prediabetes. Diabetes Care 37 (2014): 2123-2131.
- Jorde R, Figenschau Y. Supplementation with cholecalciferol does not improve glycaemic control in diabetic subjects with normal serum 25-hydroxyvitamin D levels. European Journal of Nutrition 48 (2009): 349.
- Gulseth HL, Wium C, Angel K, et al. Effects of vitamin D supplementation on insulin sensitivity and insulin secretion in subjects with type 2 diabetes and vitamin D deficiency: a randomized controlled trial. Diabetes Care 40 (2017): 872-878.
- Pilz S, Kienreich K, Rutters F, et al. Role of vitamin D in the development of insulin resistance and type 2 diabetes. Current Diabetes Reports 13 (2013): 261-270.
- Cade C, Norman AW. Rapid normalization/stimulation by 1, 25-dihydroxyvitamin D3 of insulin secretion and glucose tolerance in the vitamin D-deficient rat. Endocrinology 120 (1987): 1490-1497.
- John AN, Iqbal Z, Colley S, et al. Vitamin D receptor-targeted treatment to prevent pathological dedifferentiation of pancreatic β cells under hyperglycaemic stress. Diabetes & Metabolism 44 (2018): 269-280.
- Qureshi FM, Dejene EA, Corbin KL, et al. Stress-induced dissociations between intracellular calcium signaling and insulin secretion in pancreatic islets. Cell Calcium 57 (2015): 366-375.
- Ahn C, Lee D, Lee JH, et al. Calbindin-D9k ablation disrupt glucose/pancreatic insulin homeostasis. PloS One 11 (2016): e0164527.
- Sentsova TB, Vorozhko IV, Chernyak OO, et al. Characteristics of the Renin-Angiotensin-Aldosterone System in Carriers of Polymorphic Variants of the VDR Gene With Arterial Hypertension and Obesity. Kardiologiia (2018): 45-49.
- Wolden-Kirk H, Rondas D, Bugliani MA, et al. Discovery of molecular pathways mediating 1, 25-dihydroxyvitamin D3 protection against cytokine-induced inflammation and damage of human and male mouse islets of Langerhans. Endocrinology 155 (2014): 736-747.
- Jiang X, Peng M, Chen S, et al. Vitamin D deficiency is associated with dyslipidemia: a cross-sectional study in 3788 subjects. Current Medical Research and Opinion 35 (2019): 1059-1063.
- Wang Y, Si S, Liu J, et al. The associations of serum lipids with vitamin D status. PLoS One 11 (2016): e0165157.
- Ponda MP, Liang Y, Kim J, et al. A randomized clinical trial in vitamin D–deficient adults comparing replenishment with oral vitamin D3 with narrow-band UV type B light: effects on cholesterol and the transcriptional profiles of skin and blood. The American Journal of Clinical Nutrition 105 (2017): 1230-1238.
- Yin MT, Chan ES, Brown TT, et al. Racial Differences in Calculated Bioavailable Vitamin D with Vitamin D/Calcium Supplementation: ACTG A5280. AIDS (London, England) 31 (2017): 2337.