Chest CT Severity Score in COVID-19 at the Time of Admission and Relationship with Outcome and Duration of Admission-an Early Promising Prognostic Indicator
Article Information
Jitendra Parmar1*, Drashti Patel1, Tapan Patel1, Sandip Shah1, Manoj Singh2, Shanti Bhushan Prasad3
1Department of Radiology, Apollo Hospitals International Limited, Ahmedabad, India
2Department of Chest, Intensive and Critical Care, Apollo Hospitals International Limited, Ahmedabad,India
3Department of Intensive and Critical Care, Apollo Hospitals International Limited, Ahmedabad, India
*Corresponding author: Jitendra Parmar, Department of Radiology, Apollo Hospitals International Limited, Ahmedabad, India.
Received: 23 February 2022; Accepted: 08 March 2022; Published: 16 March 2022
Citation: Jitendra Parmar, Drashti Patel, Tapan Patel, Sandip Shah, Manoj Singh, Shanti Bhushan Prasad. Chest CT Severity Score in COVID-19 at the Time of Admission and Relationship with Outcome and Duration of Admission-an Early Promising Prognostic Indicator. Archives of Clinical and Biomedical Research 6 (2022): 277-289.
Share at FacebookAbstract
Purpose: The CT Severity Score has great significance in assessing the extent of pneumonia involvement with differentiation of mild, critical and severe types and helps clinicians achieve early diagnosis and accurate treatment.
Material and methods: 100 COVID-19 positive patients were analyzed for CT-SS and its correlation with clinical severity, laboratory markers and duration of hospital stay. The ROC curve was analyzed to obtain the optimum CT-SS threshold to discriminate patients in the common group from the patients of severe & critical groups and discriminate patients in the critical group from the patients of severe & common groups.
Results: The study comprised 57 common category, 23 severe category and 20 critical category patients. The mean chest CT-SS score was highest in critical patients (35.95), higher in severe patients (25.52) than common patients (12.18) with mean duration of admission was 13.35, 12 and 7.65 days respectively (p-value of 0.000). The optimum CT-SS threshold for discriminating patients in the common group from the patients of severe & critical groups was 21.5 with sensitivity of 93%, specificity of 86%. The optimum CT-SS threshold for discriminating patients in the critical group from the patients of severe & common groups was 28.5 with a sensitivity & specificity of 90%.
Conclusion: Initial Chest CT-SS showed significant association with duration of hospital stay and short-term prognosis of patients. Chest CT Severity Score can be used to evaluate the clinical severity of the patients on initial scans, to differentiate common, severe and critical patients and decide their management.
Keywords
COVID 19; Chest CT-SS; Hospital Stay in COVID 19 Prognostic Indicator
COVID 19 articles; Chest CT-SS articles; Hospital Stay in COVID 19 Prognostic Indicator articles
Article Details
Abbreviations
AUC: Area Under the Curve; COVID-19: Coronavirus Disease 2019; CT-SS: CT Severity Score; CT Scan: Computed Tomography Scan; CRP: C-Reactive Protein; GGO: Ground-Glass Opacities; HRCT: High-Resolution Computed Tomography; ICU: Intensive Care Unit; KV: Kilovoltage; MA: Milliamperes; MM: Millimetre; NPV: Negative Predictive Value; PPV: Positive Predictive Value; RTPCR: Real-Time Reverse Transcription-Polymerase Chain Reaction; ROC: Receiver Operating Characteristic; SARS-Cov-2: Severe Acute Respiratory Syndrome Coronavirus-2; S: Second; SD: Standard Deviation; WBC: White Blood Cell.
Units
Tube voltage: kV (Kilovoltage); Tube Current: mA (Milliamperes); WBC counts: Per cumm; CRP: mg/L; D-dimer: mcg/ml; Ferritin: ng/ml.
1. Introduction
Since December 2019, there are several cases with unknown pneumonia with similar clinical manifestations suggesting viral pneumonia appeared in Wuhan city, subsequently named the disease Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-Cov-2) [1]. World Health Organization has named the disease Coronavirus Disease 2019 (COVID-19) on February 11, 2020. This virus spreads through droplet transmission and the transmission from human to human has been remarkably high, with public health endangered globally, it was declared a pandemic disease. Diagnosis of COVID-19 depends on real-time Reverse Transcription-Polymerase Chain Reaction (RTPCR) or next-generation sequencing. The Computed Tomography (CT) / High-Resolution Computed Tomography (HRCT) scan manifestation resembles those seen in viral pneumonia. HRCT has reported high sensitivity in detecting lung infection by SARS-Cov-2 and helping the care professionals to provide better treatment [2]. The treatment methods for this disease varies according to severity among the patients. The patient with mild disease receives antiviral, symptomatic support and oxygen therapy and patients with severe disease are admitted to an intensive care unit. Most patients of COVID-19 have mild symptoms and a good prognosis [3]. However, some patients progressed from severe pneumonia to pulmonary oedema, acute respiratory distress syndrome, multiple organ failure, and death. HRCT scan has been identified as an efficient clinical diagnostic tool for patients with suspected COVID-19, monitoring disease progression, determination of disease severity and evaluating therapeutic efficacy [4]. The extent of lung involvement on HRCT scans plays a vital role in disease assessment, prognosis and follow up of patients. The CT Severity Score (CT-SS) has great significance in assessing the extent of pneumonia involvement with differentiation of mild, critical and severe types and helps clinicians achieve early diagnosis and accurate treatment [5-8]. Hence this study was conducted to evaluate the severity of COVID-19 infection and to evaluate the relationship of Chest CT-SS in COVID-19 at the time of admission with clinical severity of patient and predicting duration of admission and/or outcome.
2. Material and Methods
2.1.Ethical and Scientific Committee Approval
Ethical approval was obtained from the Institutional Review Board and Scientific Committee. The informed consent was taken as per the hospital guidelines.
2.2. Data Collection
We collected clinical and laboratory data for analysis, derived from an electronic medical record system, from July 2020 to July 2021 of patients who were confirmed to have COVID- 19 infection and underwent a chest HRCT scan on the day of admission. The results for the chest HRCT images were collected and evaluated using the Picture Archiving and Communication Systems. Initially, 215 samples were collected, out of which 115 samples were excluded from the study due to various adverse factors, including scans technically insufficient for assigning a score, negative HRCT scan for pneumonia, patients lost to follow up and patients who refused to be a part of the study. Finally, 100 patients were included in the study and subsequently statistically analysed.
2.3. HRCT Protocol
All initial chest HRCT scans were performed on the day of patients’ admission using a 128 slice CT scanner (SOMATOM; SIEMENS). Patients were placed in a supine position with a single breath-hold. Scanning parameters were as follows: scan direction (craniocaudally), tube voltage (120 kV), tube current (200-400 mA)-smart mA dose modulation, slice collimation (128×0.625mm), width (0.625×0.625mm), pitch (1), rotation time (0.5 s), and scan length (60.00–I300.00 s).
2.4. HRCT Image Analysis
Two radiologists with more than 5 years of experience evaluated the images to determine the disease severity score in each patient. The scans were first assessed whether negative or positive for typical findings of COVID-19 pneumonia (bilateral, multilobe, posterior peripheral ground-glass opacities (GGO) as defined by the RSNA Consensus statement [9]. A chest CT-SS were used to assess lung infection by COVID-19. According to the anatomical structure, the 18 segments of both lungs are divided into 20 regions, in which the apicoposterior segment of the left upper lobe is subdivided into apical and posterior segments, while the anteromedial basal segment of the left lower lobe is subdivided into anterior and medial basal segments. The lung opacities in all the 20 lung regions were subjectively be evaluated on chest CT. Depending on the parenchymal opacification of 0%, less than 50%, or equal or more than 50% of each segment region, 0, 1 and 2 scorings will be given respectively. The CT-SS is defined as the sum of the individual score in the 20 lung segment regions, which will range from 0 to 40 points [8].
2.5. Statistical analysis
The analysis was performed using Statistical Package for the Social Sciences (SPSS 21.0). Descriptive statistics of patients’ demographics, clinical, and laboratory results were reported as numbers and relative frequencies. Frequencies of CT scores were calculated and compared with other clinical variables. The Pearson correlation coefficient test and Analysis of variance (ANOVA) were used for correlations, and a p-value less than 0.05 was defined as statistically significant. The Receiver Operating Characteristic (ROC) curve analysis was for CT-SS to discriminate patients in the common group from the patients of severe & critical groups and discriminating patients in the critical group from the patients of severe & common groups and the optimal CT-SS threshold was obtained.
3. Results
100 patients were considered for the study with different clinical severity levels, comprising 57 of common category, 23 of severe category and 20 of critical category. The mean age of the common category was 50.33 years, severe was 56.70 years and the critical was 64.65 years. The overall mean age of all patients was 54.66 years with a standard deviation (SD) of 15.02. According to the gender-wise analysis, 32 patients were female, and 68 patients were male with common, severe and critical illness were 65.6%, 9.4% and 25% respectively in female patients and 52.9%, 29.4% and 17.6% respectively in male patients. Fever was the main symptom in 73 patients, followed by weakness in 51 patients and cough in 49 patients. Fever, weakness, sore throat and dysgeusia were more common in the common category while cough was more common in the severe category and dyspnoea in critical patients. Adverse respiratory signs were more common in critical category patients. Severe and critical patients required oxygen supplementation. 19 out of 20 critical patients were supported with mechanical ventilation admitted to the Intensive Care Unit (ICU). Complications such as shock and multiple organ failure were observed in these patients. Inflammatory markers were significantly raised (p-value – 0.000) in severe and critical category patients as compared to common category patients. Mean White Blood Cell (WBC) counts (per cumm) were 7464.09, 10219.22 and 12894.95 in common, severe and critical category patients. In addition, 36.72, 118.52 and 187.10 were mean C-Reactive Protein (CRP) values (mg/L), 0.42, 1.64, 3.93 were mean D-dimer values (mcg/ml), 232.25, 557.48, 1479.80 were mean ferritin values (ng/ml) identified for common, severe and critical categories respectively. In addition, the mean C-Reactive Protein (CRP), mean Ferritin and D- DIMER were highest in critical patients (187.10, 1479.80, and 3.93 respectively), higher in severe patients (118.2, 557.48 and 1.64 respectively) than common patients (36.72, 232.25 and 0.42 respectively). As per the analysis, 46 patients had diabetes mellitus, 45 patients had hypertension and 10 patients had cardiovascular disease. The detailed demographic and clinical data of 100 patients are summarized in (Table 1).
|
Clinical Severity |
|||||
|
Common |
Severe |
Critical |
Total |
P - Value |
|
|
Total Patients |
57 |
23 |
20 |
100 |
|
|
Mean Age in Years (SD*) |
50.33 (14.39) |
56.7 (15.26) |
64.65 (11.55) |
54.66 (15.02) |
0.003 |
|
Signs and Symptoms |
|||||
|
Fever |
33 |
22 |
18 |
73 |
< 0.05 |
|
Cough |
15 |
18 |
16 |
49 |
< 0.05 |
|
Dyspnoea |
13 |
13 |
17 |
43 |
< 0.05 |
|
Weakness |
28 |
11 |
12 |
51 |
0.499 |
|
Sore Throat |
17 |
4 |
0 |
21 |
0.022 |
|
Dysgeusia |
15 |
3 |
2 |
20 |
0.222 |
|
Diarrhoea |
17 |
2 |
1 |
20 |
0.023 |
|
Headache |
9 |
1 |
5 |
15 |
0.138 |
|
RR ≥30 breaths/ min * |
0 |
14 |
19 |
33 |
< 0.05 |
|
SpO2 ≤93% at rest * |
0 |
23 |
19 |
42 |
< 0.05 |
|
(PaO2)/(FiO2 ≤300mmHg * |
0 |
0 |
19 |
19 |
< 0.05 |
|
Shock |
0 |
0 |
19 |
19 |
< 0.05 |
|
Organ failure that requires ICU care |
0 |
0 |
19 |
19 |
< 0.05 |
|
Respiratory Failure and Requiring Mechanical Ventilation |
0 |
0 |
19 |
19 |
< 0.05 |
|
Mean Inflammatory Markers (SD) |
|||||
|
WBC (/cumm) * |
7464.09 (1360.99) |
10219.22 (3910.27) |
12894.95 (3682.81) |
--- |
< 0.05 |
|
CRP (mg/L) * |
36.72 (39.31) |
118.52 (86.07) |
187.1 (116.66) |
--- |
< 0.05 |
|
D-DIMER (mcg/ml) |
0.42 (0.52) |
1.64 (1.78) |
3.93 (2.30) |
--- |
< 0.05 |
|
Ferritin (ng/ml) |
232.25 (90.84) |
557.48 (393.37) |
1479.8 (1310.01) |
--- |
< 0.05 |
|
Mean Duration of Symptoms in Days (SD) |
6.63 (2.83) |
7.7 (3.08) |
9.55 (2.68) |
--- |
--- |
|
Co-morbidities |
|||||
|
Cardiovascular Disease |
4 |
1 |
5 |
10 |
--- |
|
Diabetes Mellitus |
21 |
11 |
14 |
46 |
--- |
|
Hypertension |
19 |
13 |
13 |
45 |
--- |
|
Chronic Lung Disease |
1 |
1 |
4 |
6 |
--- |
|
Cancer |
1 |
1 |
1 |
3 |
|
|
Chronic Kidney Disease |
1 |
1 |
4 |
6 |
--- |
|
Hypothyroidism |
3 |
1 |
1 |
5 |
--- |
|
Smoking |
2 |
2 |
4 |
8 |
--- |
|
Mean Duration of Admission in Days (SD) |
7.65 (1.18) |
12 (1.97) |
13.35 (4.33) |
--- |
< 0.05 |
|
*SD – Standard Deviation, RR – Respiratory Rate, SpO2 – Oxygen Saturation, PaO2/FiO2 – a ratio of arterial oxygen partial pressure (PaO2 in mmHg) to fractional inspired oxygen (FiO2 expressed as a fraction, not a percentage), WBC – White Blood Cells, CRP – C- Reactive Protein |
|||||
Table 1: Demographic and Clinical Data of 100 patients with COVID-19 Pneumonia
The analysis of HRCT findings has shown that GGO were the most common finding in 95 patients followed by interstitial septal thickening in 55 patients and consolidation in 51 patients. All the common and severe patients had ground-glass opacities. 30 out of 57 patients of common category patients had GGO along with interstitial septal thickening suggestive of Crazy Paving pattern (Figure 1). Combination of GGO and consolidations were more common in severe category patients (Figure 2). The combination of GGO, consolidation, vascular as well as bronchial dilatation, architectural distortion and pleural effusion were common in critical patients.
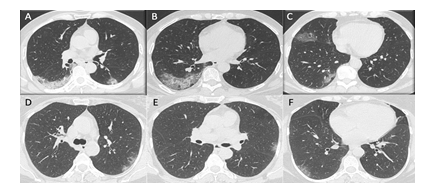
Figure 1: HRCT chest of two patients of Common Category: A, B and C show multifocal areas of GGO and Crazy Paving patterns, predominantly in peripheral distribution with CT- SS of 8/40 in 42 years old male patient, who was discharged in stable condition after 6 days of hospital stay. D, E and F show multifocal patchy GGO with peripheral distribution and CT-SS of 6/40 in 79 years old female patient, who was discharged in a stable condition after 7 days of hospital stay.
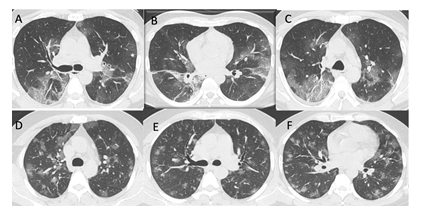
Figure 2: HRCT chest of two patients of Severe Category: A, B and C show multifocal areas of GGO, Crazy Paving patterns and few areas of consolidations, predominantly in peripheral distribution with CT-SS of 22/40 in 55 years old male patient, who was discharged in stable condition after 10 days of hospital stay. D, E and F show multifocal patchy GGO with peripheral distribution and CT-SS of 28/40 in 79 years old male patient, who was discharged in a stable condition after 12 days of hospital stay.
Peripheral and bilateral ground-glass densities are more common in common patients, while diffuse (peripheral as well as peribronchovascular) combination of densities, including predominant consolidation, ground-glass opacities interspersed with interstitial septal thickening and dilatation of vascular as well as bronchial dilatation with architectural distortion were more common in critical patients (Figure 3). The detail of HRCT findings is summarized in Table 2.
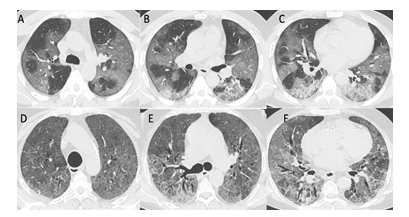
Figure 3: HRCT chest of two patients of critical Category: A, B and C show multifocal areas of discrete and confluent GGO, Crazy Paving patterns and few areas of consolidations, diffusely scattered in both lung parenchyma with CT-SS of 30/40 in 46 years old male patient, who was discharged in stable condition after 15 days of hospital stay. D, E and F show diffuse GGO with interstitial septal thickening, a crazy-paving pattern associated bronchial dilatation and early architectural distortion, with CT-SS of 40/40 in 58 years old female patient, who died after 16 days of admission.
|
Clinical Severity |
|||||
|
Common |
Severe |
Critical |
Total |
P -Value |
|
|
Total Patients |
57 |
23 |
20 |
100 |
|
|
HRCT Scan Findings |
|||||
|
GGO** |
57 |
23 |
15 |
95 |
< 0.05 |
|
GGO + consolidation |
16 |
21 |
11 |
48 |
< 0.05 |
|
Consolidation |
16 |
20 |
15 |
51 |
< 0.05 |
|
Crazy Paving |
30 |
12 |
11 |
53 |
0.893 |
|
Atol Sign |
4 |
7 |
6 |
17 |
0.007 |
|
Vacuolar sign |
7 |
6 |
3 |
16 |
0.3 |
|
Microvascular dilation |
7 |
7 |
11 |
25 |
< 0.05 |
|
Air bronchogram |
7 |
9 |
11 |
27 |
< 0.05 |
|
GGO |
58 |
23 |
15 |
96 |
< 0.05 |
|
GGO + consolidation |
16 |
21 |
11 |
48 |
< 0.05 |
|
Consolidation |
16 |
20 |
15 |
51 |
< 0.05 |
|
Crazy Paving |
30 |
12 |
11 |
53 |
0.893 |
|
Atol Sign |
4 |
7 |
6 |
17 |
0.007 |
|
Vacuolar sign |
7 |
6 |
3 |
16 |
0.3 |
|
Microvascular dilation |
7 |
7 |
11 |
25 |
< 0.05 |
|
Air bronchogram |
7 |
9 |
11 |
27 |
< 0.05 |
|
Septal thickening |
30 |
13 |
12 |
55 |
0.676 |
|
Thickening of pleura |
4 |
3 |
6 |
13 |
0.021 |
|
Pleural retraction |
6 |
1 |
5 |
12 |
0.078 |
|
Pleural effusion |
2 |
6 |
12 |
20 |
< 0.05 |
|
Subpleural line |
10 |
2 |
9 |
21 |
0.005 |
|
Bronchus distortion |
1 |
2 |
10 |
13 |
< 0.05 |
|
Fibrotic strips |
7 |
4 |
13 |
24 |
< 0.05 |
|
Architecture distortion |
1 |
2 |
10 |
13 |
< 0.05 |
|
Opacity (Axial) Distribution |
|||||
|
Central (peribronchovascular) |
31 |
21 |
19 |
71 |
< 0.05 |
|
Peripheral |
58 |
23 |
19 |
100 |
< 0.05 |
|
Bilateral lung disease |
52 |
23 |
19 |
94 |
< 0.05 |
|
** GGO – Ground Glass Opacities |
|||||
Table 2: HRCT Findings in 100 patients with COVID-19 pneumonia
The mean chest CT-SS score was significantly higher in critical patients (35.95), higher in severe patients (25.52) than common patients (12.18) with a p-value of 0.000. The mean duration of admission was 7.65 days in common patients, 12.00 days in severe patients and 13.35 days was in critical patients (p-value of 0.000). The CT-SS and duration of admission were statistically compared, it was found that the CT-SS had a significant correlation with duration of admission, with a p-value of 0.000 (Table 3). More the CT-SS more was the duration of admission and increased the risk of complications. In this study, the mortality was 18 out of 100, and all of them were critical category patients. There was no mortality in common and severe patients, while only 2 out of 20 critical patients could survive, who were discharged after 25 and 30 days of admission.
|
Clinical Severity |
|||||
|
Common |
Severe |
Critical |
Total |
P- Value |
|
|
Total Patients |
57 |
23 |
20 |
100 |
|
|
Mean Duration of Symptoms in Days (SD) |
6.63 (2.83) |
7.7 (3.08) |
9.55 (2.68) |
--- |
--- |
|
Mean Duration of Admission in Days (SD) |
7.65 (1.18) |
12 (1.97) |
13.35 (4.33) |
--- |
< 0.05 |
|
Mean Chest CT-SS*** (SD) |
12.18 (6.48) |
25.52 (4.38) |
35.95 (4.61) |
20 (11.22) |
< 0.05 |
|
*** CT-SS - Computed Tomography-Severity Score |
|||||
Table 3: Comparison of mean duration of admission and CT-SS in COVID-19 patients
The Receiver Operating Characteristic (ROC) curve analysis for CT-SS is shown in Figure 4. The Area Under The Curve (AUC) for discriminating patients in the common group from the patients of severe & critical groups (Figure 4A) was 0.960 (standard error, 0.017; 95% confidence interval: 0.927, 0.993) and the optimal CT-SS threshold was 21.5 with a sensitivity of 93%, specificity of 86%, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of 90%. The AUC for discriminating patients in the critical group from the patients of severe & common groups (Figure 4B) was 0.976 (standard error, 0.019; 95% confidence interval: 0.938, 1.0) and the optimal CT-SS threshold was 28.5 with sensitivity & specificity of 90%, PPV of 69.2% and NPV of 97.3%.
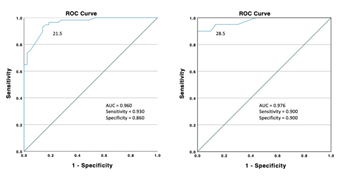
Figure 4: ROC curve analysis. A) The area under the curve for discriminating patients in the common group from the patients of severe & critical groups. B) The area under the curve for discriminating patients in the critical group from the patients of severe & common.
4. Discussion
COVID-19 infection is characterized by a systemic inflammatory response that affects the lungs, blood, digestive system, and circulatory systems. The study by Tsamakis et al. [10] has suggested that 64% of patients affected by the virus were found with pulmonary manifestations. The clinical presentation varies from asymptomatic carrier to patients requiring assisted ventilatory support and ICU admission with increased mortality. In addition to this, patients who are having heart disease and Asthma were affected the most. The HRCT scan helps to provide the extent of pulmonary involvement and triage of the patients in need of hospital admission accordingly. In the current study, 100 patients were considered for the study who fulfilled inclusion criteria. Among all patients, 57 patients were in common (57 %), 23 patients were in severe (23%), and 20 patients were in the critical (20%) category. From the analysis of the current study, it is observed that patients in common patients were having a lower age group than severe and critical patients. The mean age was 50.33 years for common patients, 56.70 years for severe patients and 64.65 years for critical patients. The overall mean age of all patients was 54.66 years. Among all patients, 68 were male patients and 32 were female patients. Patients in the common category presented early with less duration of symptoms than severe and critical categories. The mean duration of symptoms for the common patient was 6.63 days, 7.70 days for severe and 9.55 days for critical patients (p-value <0.05). The patients presented most with fever followed by weakness, cough and dyspnoea. 73 patients were having fever, 51 patients were having weakness and 49 patients were having cough. 15 patients presented with headache, 20 patients with diarrhoea and dysgeusia and 21 patients with a sore throat. Diabetes and hypertension were the most common co- morbidities. 46 patients were found with diabetes mellitus, 45 patients were having hypertension and 10 patients were having cardiovascular disease. 8 patients were smokers, 6 patients were having chronic kidney and chronic lung disease. Bhandari et al. [11] in their study observed that Diabetes mellitus, hypertension, chronic obstructive pulmonary disease and coronary artery disease were major comorbidities. These patients had a more symptomatic presentation of COVID-19. HRCT chest in COVID-19 patients had a major diagnostic and prognostic importance as positive HRCT findings were more prominent in symptomatic patients and co-morbid patients. Saleemi et al. [7] in their study of RTPCR confirmed 29 patients found that bilateral ground- glass opacities were the most common CT scan feature in patients with COVID-19 (76%). Opacities were dominant in the lower zone (72%) and frequently distributed peripherally (48%). Severe disease was most likely to have bilateral opacities compared with mild disease. As per the outcome of the current study, on CT Chest evaluation, the ground glass opacities were commonly found with the predominant peripheral distribution. 71 % had central as well as peripheral distribution considering all categories. Common patients who presented early had patchy areas of ground-glass opacities involving unilateral or bilateral lung fields. Severe and critical patients who presented later showed ground-glass opacities and consolidations diffusely involving bilateral lung parenchyma. Along with it, septal thickening was seen in 55%, crazy paving appearance in 53 %, consolidation in 51%. Findings like pleural effusion, fibrotic bands, vascular dilatation, bronchus and architecture distortion were found more common in critical patients. According to a study by Francone et al. [6], CT score was significantly higher in critical and severe than in mild stage and among late-phase than early-phase patients (p < 0.0001). CT score was significantly correlated with CRP and D-dimer levels. The current study has also analyzed that CT-SS was higher in critical and severe patients compared to common patients, with a mean CT-SS of 12.18/40 for common, 25.52/40 for severe and 35.95/40 for common patients (p-value < 0.05). CRP and D-dimer levels were high in critical and severe patients compared to common patients with a mean CRP and D-dimer values, 187.10 and 3.93 for critical, 118.52 and 1.64 for severe and 36.72 and 0.42 for common patients respectively. CT- SS showed a positive correlation with inflammatory markers and clinical severity. Bhandari et al. [11] in their study concluded that CT-SS was correlated with the clinical status of the patients, mild cases were showing < 15/25 score in 45.83% and severe cases were showing >15/25 score in 87.50% patients. Yang et al. [8] have analyzed that CT-SS were higher in the severe COVID-19 cases compared to mild cases (P>0.05) and the optimal CT- SS threshold for finding the severe COVID-19 was 19.5/40 (curve was 0.892) with 83.3% sensitivity and 94% specificity. In the present study, the area under the curve for discriminating patients in the common group from the patients of severe & critical groups was 0.960 (standard error, 0.017; 95% confidence interval: 0.927, 0.993) and the optimal CT-SS threshold was 21.5/40 with a sensitivity of 93%, specificity of 86%, positive predictive value (PPV) and Negative Predictive Value (NPV) of 90%. The area under the curve for discriminating patients in the critical group from the patients of severe & common groups (Figure B) was 0.976 (standard error, 0.019; 95% confidence interval: 0.938, 1.0) and the optimal CT-SS threshold was 28.5/40 with sensitivity & specificity of 90%, Positive Predictive Value (PPV) of 69.2% and Negative Predictive Value (NPV) of 97.3%. Saeed et al. [12] in the comparative study of Chest CT Severity score with clinical severity in patients of COVID-19 analyzed that CT-SS show a positive correlation with inflammatory lab markers, length of hospital stays and hospital requirement. Similar findings observed in the current study, critical patients had longer hospital duration stay with poor outcomes and higher mortality. CT-SS was higher in such patients. Oxygen requirement and need for mechanical ventilation were commonly seen with more complications such as acute respiratory distress syndrome, shock, and multiple organ failure. The mean duration of hospital stay was 7.65 for common patients, 12.0 for severe patients, 13.35 for critical patients. The mean duration of admission in critical patients is still under-documented as the mortality was very high in critical patients (90%) Common patients had lower CT-SS, lesser hospital duration stays, and they recovered well while severe patients had an intermediate duration of hospital stay, higher CT-SS and required oxygen supplementation.
Francone et al. [6] concluded that a CT score of ≥ 18/25 was associated with increased mortality and was found to be predictive of death. The current study observed a similar scenario and corresponding to the current study, CT-SS > 28.5/40 was associated with increased mortality. All the mortality of 18 patients were from the critical category. The main reason was the late presentation and high CT-SS at the time of admission (p < 0.05). Out of 82 survived patients, 69.5% were from common, 28.0 % were from severe and only 2.4 % were from the critical category. Common patients had a good survival rate while critical patients showed significant mortality. A similar kind of study was conducted by Bellos et al. [13] on 42 patients, which showed a similar conclusion, stating the threshold of 10.5/25 for the prediction of admission to the ICU with sensitivity and specificity of 75% and 70% respectively. In contrast, Zayed et al. [14] concluded in a retrospective study on 142 patients that CT-SS score of less than 7.5/40 and CO-RADS less than 4.5 could rule out severe COVID-19 disease. The optimal CT-SS threshold for identifying common patients was 21.5/40 and 28.5/40 for critical patients. The number of patients with CT-SS < 21.5/40 was 59, among them 53 were from the common category, 1 from the critical category and 5 from the severe category. CT-SS < 21.5 could rule out severe and critical patients with sensitivity and specificity of 93% and 86% respectively. The positive and negative predictive values were 90%. The number of patients with CT-SS > 28.5/40 was 26, among them 18 from a critical category, 7 from severe category and 1 from common category. CT-SS < 28.5 could rule out critical patients with sensitivity and specificity of 90% (p < 0.05). The PPV and NPV were 69% and 97% respectively. The ROC curve analysis suggested CT-SS has high sensitivity in identifying common and critical patients. The chest CT score is a good indicator of the extent of systemic inflammation. The extent of lung involvement on CT scans plays a vital role in disease assessment, prognosis and follow up of patients. The CT-SS has great significance in assessing the extent of pneumonia involvement with differentiation of common, severe and critical types and helps clinicians achieve early diagnosis and accurate management.
5. Conclusion
The current study suggests that Chest CT-SS is a useful tool for the initial evaluation of COVID- 19 patients. It can be used for triage purposes of COVID-19 patients in need of a hospital, especially during the peak of the pandemic wave. It has high sensitivity in differentiating critical patients and planning their management accordingly. It showed a positive correlation with inflammatory markers such as CRP, D-dimer, Ferritin. Initial Chest CT-SS showed significant association with duration of hospital stay and short and long-term prognosis with the outcome of patients. Lower CT-SS was associated with good outcomes while more death rates were observed in critical patients with higher CT-SS. In conclusion, Chest CT Severity Score can be used to evaluate the clinical severity of the patients on initial scans, to differentiate common, severe and critical patients and decide their management.
Limitations
Patients who did not have any opacity in the initial Chest CT scan were not included in the study. Data of only admitted patients were collected, patients who visited on an OPD basis and managed by home care were not included in the study. Chest CT-SS was calculated by a small group of experienced radiologists, however, the consistency of CT-SS among readers should be researched further.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and necessary Institutional Scientific Committee and ethics committee approvals have been obtained. All necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived.
Competing Interest Statement
The authors have declared no competing interest.
Clinical Trial
Retrospective study
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Zhao W, Zhong Z, Xie X, et al. Relation between chest CT findings and clinical conditions of coronavirus disease (covid-19) pneumonia: A multicenter study. Am J Roentgenol 214 (2020): 1072-1077.
- Kwee TC, Kwee RM. Chest CT in covid-19: What the radiologist needs to know. Radiographics 40 (2020): 1848-1865.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J Am Med Assoc 323 (2020): 1061-1069.
- Figliozzi S, Masci PG, Ahmadi N, et al. Predictors of adverse prognosis in COVID-19: A systematic review and meta-analysis. Eur J Clin Invest 50 (2020): 1-15.
- Hafez MAF. The mean severity score and its correlation with common computed tomography chest manifestations in Egyptian patients with COVID-2019 pneumonia. Egypt J Radiol Nucl Med 51 (2020): 254.
- Francone M, Iafrate F, Masci GM, et al. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol 30 (2020): 6808-6817.
- Saleemi S, Skaff F, Albaiz F, et al. Radiology Features of Chest Imaging and Its Correlation to Clinical Severity in Patients with COVID-19. Int J Med Imaging 8 (2020): 35-38.
- Yang R, Li X, Liu H, et al. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiol Cardiothorac Imaging 2 (2020): 200047.
- Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging 35 (2020): 219-227.
- Tsamakis K, Rizos E, Manolis A, et al. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med 19 (2020): 3451-3453.
- Bhandari S, Singh A, Bagarhatta M, et al. Evaluation of clinico–Radiological profile and correlation with ultrasonography of the chest in coronavirus disease 2019 pneumonia. Indian J Med Spec 11 (2020): 70-75.
- Saeed GA, Gaba W, Shah A, et al. Correlation between Chest CT Severity Scores and the Clinical Parameters of Adult Patients with COVID-19 Pneumonia. Radiol Res Pract 6 (2021): 6697677.
- Bellos I, Tavernaraki K, Stefanidis K, et al. Chest CT severity score and radiological patterns as predictors of disease severity, ICU admission, and viral positivity in COVID-19 patients. Respir Investig 59 (2021): 436-445.
- Zayed NE, Bessar MA, Lutfy S. CO-RADS versus CT-SS scores in predicting severe COVID-19 patients: retrospective comparative study.Egypt J Bronchol(2021): 13
