Chest CT Scan In Patients With Contusion and COVID-19, A Comparative Study With Pure Lung Contusion
Article Information
Amin Sadraei M.D.1, Seyed Hamed Jafari M.D.2, Seyed Mehdi Shahnematollahi M.D.3 Mohammadamir Taherinezhad M.D.4, Nazanin Sadraei M.D.5*, Zahra Hooshanginezhad M.D.6
1Shiraz Nephro-Urology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
2Associated professor of radiology, Shiraz University of Medical Science. Medical Imaging Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
3School of medicine, Shiraz University of Medical Science, Shiraz, Iran
4Cardiology resident, School of Medicine, Department of cardiology, Shiraz University of Medical Sciences, Shiraz, Iran
5Medical Imaging Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
6Shiraz University of Medical Sciences, Shiraz, Iran
*Corresponding Author: Nazanin Sadraei M.D.
Received: 10 February 2023; Accepted: 20 February 2023; Published: 16 March 2023
Citation: Amin Sadraei M.D., Seyed Hamed Jafari M.D., Seyed Mehdi Shahnematollahi M.D. Mohammadamir Taherinezhad M.D., Nazanin Sadraei M.D., Zahra Hooshanginezhad M.D. Chest CT scan in patients with contusion and COVID-19, a comparative study with pure lung contusion. Journal of Radiology and Clinical Imaging. 6 (2023): 41-47.
Share at FacebookAbstract
Resource allocation for traumatic patients who are positive/negative for COVID-19 challenges the diagnosis. This study aims to compare the chest CT of COVID-19 associated with lung contusion versus those with lung contusion only. CT-scans of 9 RT-PCR positive patients with lung contusion due to MVA (CC group) and 16 patients with lung contusions from pre-COVID-19 (CO group) were revaluated. The distribution and characteristics of presenting CT-scan findings; including presence, shape, distribution of GGO, consolidations, subpleural sparing, crazy-paving and Atoll sign. Presence of effusions and cavities were compared. Time course of the opacities was compared. Bilateral distribution of opacities was noted in 100% of CC and 87.5% of CO group. There was no significant difference between GGO or consolidation shapes (P=0.44 and P=0.66). Both GGO and consolidations were more diffusely distributed in CC, a predominantly peripheral distribution was more commonly seen in the CO group (P=0.03 and P=0.01). Subpleural sparing was noted in 93.8% of CO as compared to 44% of CC group (p=0.04). Time to resolution was significantly longer in CC (15±6days) comparing to CO patients (P=0.02). 'Typical' chest CT findings including bilateral peripheral GGO and consolidations, crazypaving, Atoll signs and also less typical findings e.g. subpleural sparing is seen in lung contusion and COVID-19 pneumonitis. Lesion Time course might be a better radiologic discriminator between the two entities.
Keywords
: COVID-19; lung contusion; Chest CT scan; RT-PCR
COVID-19 articles; lung contusion articles; Chest CT scan articles; RT-PCR articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals lung contusion articles lung contusion Research articles lung contusion review articles lung contusion PubMed articles lung contusion PubMed Central articles lung contusion 2023 articles lung contusion 2024 articles lung contusion Scopus articles lung contusion impact factor journals lung contusion Scopus journals lung contusion PubMed journals lung contusion medical journals lung contusion free journals lung contusion best journals lung contusion top journals lung contusion free medical journals lung contusion famous journals lung contusion Google Scholar indexed journals Chest CT scan articles Chest CT scan Research articles Chest CT scan review articles Chest CT scan PubMed articles Chest CT scan PubMed Central articles Chest CT scan 2023 articles Chest CT scan 2024 articles Chest CT scan Scopus articles Chest CT scan impact factor journals Chest CT scan Scopus journals Chest CT scan PubMed journals Chest CT scan medical journals Chest CT scan free journals Chest CT scan best journals Chest CT scan top journals Chest CT scan free medical journals Chest CT scan famous journals Chest CT scan Google Scholar indexed journals RT-PCR articles RT-PCR Research articles RT-PCR review articles RT-PCR PubMed articles RT-PCR PubMed Central articles RT-PCR 2023 articles RT-PCR 2024 articles RT-PCR Scopus articles RT-PCR impact factor journals RT-PCR Scopus journals RT-PCR PubMed journals RT-PCR medical journals RT-PCR free journals RT-PCR best journals RT-PCR top journals RT-PCR free medical journals RT-PCR famous journals RT-PCR Google Scholar indexed journals ground glass opacities articles ground glass opacities Research articles ground glass opacities review articles ground glass opacities PubMed articles ground glass opacities PubMed Central articles ground glass opacities 2023 articles ground glass opacities 2024 articles ground glass opacities Scopus articles ground glass opacities impact factor journals ground glass opacities Scopus journals ground glass opacities PubMed journals ground glass opacities medical journals ground glass opacities free journals ground glass opacities best journals ground glass opacities top journals ground glass opacities free medical journals ground glass opacities famous journals ground glass opacities Google Scholar indexed journals lactate dehydrogenase articles lactate dehydrogenase Research articles lactate dehydrogenase review articles lactate dehydrogenase PubMed articles lactate dehydrogenase PubMed Central articles lactate dehydrogenase 2023 articles lactate dehydrogenase 2024 articles lactate dehydrogenase Scopus articles lactate dehydrogenase impact factor journals lactate dehydrogenase Scopus journals lactate dehydrogenase PubMed journals lactate dehydrogenase medical journals lactate dehydrogenase free journals lactate dehydrogenase best journals lactate dehydrogenase top journals lactate dehydrogenase free medical journals lactate dehydrogenase famous journals lactate dehydrogenase Google Scholar indexed journals erythrocyte sedimentation rate articles erythrocyte sedimentation rate Research articles erythrocyte sedimentation rate review articles erythrocyte sedimentation rate PubMed articles erythrocyte sedimentation rate PubMed Central articles erythrocyte sedimentation rate 2023 articles erythrocyte sedimentation rate 2024 articles erythrocyte sedimentation rate Scopus articles erythrocyte sedimentation rate impact factor journals erythrocyte sedimentation rate Scopus journals erythrocyte sedimentation rate PubMed journals erythrocyte sedimentation rate medical journals erythrocyte sedimentation rate free journals erythrocyte sedimentation rate best journals erythrocyte sedimentation rate top journals erythrocyte sedimentation rate free medical journals erythrocyte sedimentation rate famous journals erythrocyte sedimentation rate Google Scholar indexed journals reversed halo sign articles reversed halo sign Research articles reversed halo sign review articles reversed halo sign PubMed articles reversed halo sign PubMed Central articles reversed halo sign 2023 articles reversed halo sign 2024 articles reversed halo sign Scopus articles reversed halo sign impact factor journals reversed halo sign Scopus journals reversed halo sign PubMed journals reversed halo sign medical journals reversed halo sign free journals reversed halo sign best journals reversed halo sign top journals reversed halo sign free medical journals reversed halo sign famous journals reversed halo sign Google Scholar indexed journals CT Scan articles CT Scan Research articles CT Scan review articles CT Scan PubMed articles CT Scan PubMed Central articles CT Scan 2023 articles CT Scan 2024 articles CT Scan Scopus articles CT Scan impact factor journals CT Scan Scopus journals CT Scan PubMed journals CT Scan medical journals CT Scan free journals CT Scan best journals CT Scan top journals CT Scan free medical journals CT Scan famous journals CT Scan Google Scholar indexed journals Imaging articles Imaging Research articles Imaging review articles Imaging PubMed articles Imaging PubMed Central articles Imaging 2023 articles Imaging 2024 articles Imaging Scopus articles Imaging impact factor journals Imaging Scopus journals Imaging PubMed journals Imaging medical journals Imaging free journals Imaging best journals Imaging top journals Imaging free medical journals Imaging famous journals Imaging Google Scholar indexed journals
Article Details
1. Introduction
New coronavirus disease (COVID-19) is one of the most recent catastrophes of modern-day human history. First case of COVID-19 emerged in December 2019 in the city of Wuhan located in Hubei province in China, with drastic increase in number of cases of a severe respiratory disease [1]. This contagious virus spread rapidly around the globe. During this pandemic, Iran was not an exception as the first positive case was formally reported on February 1st, 2020[2]. At the time of this investigation Iran ranked the fourteenth country in prevalence and ninth country in the number of deceased cases. Besides, Iran is ranked as the fifth country in traffic accidents with prevalence about twenty times higher than the global average [3]. Thoracic injury is the third common injuries after head and extremities.
Patients with COVID-19 classically present with symptoms such as fever (98%), cough (76%), dyspnea (55%) and myalgia or fatigue (44%), and less commonly with symptoms such as productive cough and rarely hemoptysis [4]. Subclinical COVID-19 has been reported in numbers of cases [5]. The diagnosis of COVID-19 may be confirmed with 30-60 % sensitivity by reverse-transcription polymerase chain reaction (RT-PCR) or gene sequencing of respiratory or blood specimens [6]. According to low sensitivity of RT-PCR and its limited availability in many communities, typical computed tomography (CT) scan findings in the proper clinical setting have been used as preliminary diagnostic tool in some countries. CT-scan is however not considered to be a proper screening method, given the fact that it can be negative in up to 50% of patients in the first two days since onset of the symptoms.
Most typical findings seen in the chest CT-scan include ground glass opacities (GGO) and consolidation with bilateral, peripheral, posterior and basal predilection, crazy paving appearance, and atoll sign. Some of the atypical appearances that have been reported infrequently in CT-scans include mediastinal lymphadenopathy, tree-in-bud appearance, pleural effusion, cavitation and pneumothorax [7-9].
For the evaluation of thoracic injuries, CT-scan imaging is considered as the gold standard of diagnosis. The spectrum of abnormalities comprise of pneumothorax, hemothorax, pulmonary contusion and laceration and injuries to the airways [10,11]. Lung laceration manifests as round or oval cavities containing blood or air (hematocele, pneumatocele and hematopneumatocele) with unilocular and multilocular appearance. CT-scan findings of pulmonary contusion are made up of nonsegmental patchy air space opacities, GGOs and consolidation with ill-defined borders with sparing of subpleural space predominant in basal and posterior parts of lung field [12,13].
This overlap in findings and the frequent occurrence of asymptomatic patients in the population, along with the higher mortality rate of hospital acquired COVID-19 in the medical staff has led to a concern for how to manage lung opacities [14].
The objective of this study was to compare the chest CT findings in patients with RT-PCR- proven COVID-19 detected after hospital admission for lung contusion with patients having lung contusion in the pre-COVID-19 era.
2. Materials and Methods
2.1 Patient collection and data resources
This retrospective observational study included a total of 25 patients. Nine patients with motor- vehicle-accidents during one year diagnosed as COVID-19 by RT-PCR test (Table 1) having contusion were grouped as COVID-19 contusion group (CC group). At the time of admission, patients suffering from blunt major trauma and suspicious findings in their Chest-X-Ray underwent additional chest CT-scan. The possibility of recently emerging COVID-19 was considered for the patients with suspicious CT-scans and those who developed typical symptoms during their hospital stay. Suspicious symptoms are included fever, leukocytosis, lymphopenia and rise of serum inflammatory markers such as lactate dehydrogenase (LDH), C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Diagnosis of COVID-19 was made in all cases by one of the two fellowship-trained infectious disease specialists of the hospital. Follow up CT-scan was performed in all cases within five to ten days after the initial CT. In all patients RT-PCR tests were performed using nasopharyngeal swabs taken [15]. The control group (Contusion only or CO group) included first 16 consecutive patients with motor vehicle accidents starting at November first 2019 who had a diagnosis of lung contusion based on hospital records. All patients (CO and CC) had at least two CT-scans during their hospital stay, no less than three days apart.
|
demographics |
CC patients |
CO patients |
|
Sex |
||
|
Male |
8 |
13 |
|
Female |
1 |
3 |
|
Age |
||
|
Mean |
41.9 |
32.4 |
|
Standard deviation |
14.9 |
10.6 |
|
Range |
18-62 |
17-54 |
Table 1: Patients’ characteristics
2.2 Imaging techniques
All images included were obtained by Bright speed 16 (GE medical systems, Milwaukee, WI, United States). Scanning parameters were: tube voltage: 100-120 kVp, tube current modulation (50-100 mAs), pitch: 0.8-1.5 matrix: 512*512 slice thickness: ten mm, field of view of 350 mm*350 mm.
2.3 Image analysis
CT-scans were reviewed by three radiologists with 15, 12 and two years of experience. When discordant the difference of opinion was resolved by a third reader. Chest CT-scan findings of all patients were evaluated for presence of GGO, consolidation, distribution of findings (single, multiple, peripheral, central, or diffuse pattern), round, and/or irregular shape opacities, crazy paving pattern, the reversed halo sign, presence of reticular lines, subpleural sparing, pleural effusion, rib fracture, pneumothorax, and cavitation using a standard form. The CC and CO groups were anonymized and reported without knowledge of the date of the exam or patient symptoms on an offline DICOM reader (Kpacs).
This study was approved by our institutional ethics committee. Informed consent was waived for this anonymized retrospective study.
2.4 Statistical analysis
The data was analyzed by SPSS software. Chi-square goodness of fit test was used to compare the frequencies. P-values of less than 0.05 were considered as statistically significant (SPSS version 15.0 SPSS, IBM, NY, USA).
3. Results
A total of 25 patients, including 21 males and four females (mean age 35.8±12.9 years; age range 17-62 years).
3.1 Lung opacities
Multiple GGOs were observed in both groups except for one of the CC group. The difference was significant between two groups (p =0.036; Table 2). Multiple consolidations were noted in both groups with no significant difference (p=0.339) Shape of lung opacities, either consolidations or GGOs, were not significantly different between the two groups. Round and/or irregular shape opacities were present in both groups (Figure 1and 2). Crazy paving appearance (Figure 3) was noted in two cases in the CO while single case in the CC group showed this pattern (p= 0. 0.918). The “reversed halo sign” (as defined by central GGO with a rim of at least two mm thick consolidation surrounding most of its circumference) (Figure 4) was noted in two of the CO and none of CC patients
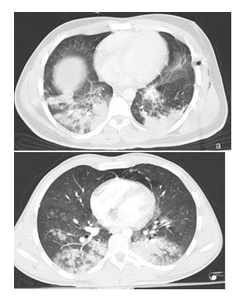
Figure 1: Axial slices of Chest CT scans at level of the heart a) an 18 y/o male with MVA in from pre-COVID-19 era with multiple irregular and round shaped consolidations. And b) a 22 y/o male with MVA and lung Contusion and COVID-19 infection also with multiple irregular and round shape consolidations and GGO.
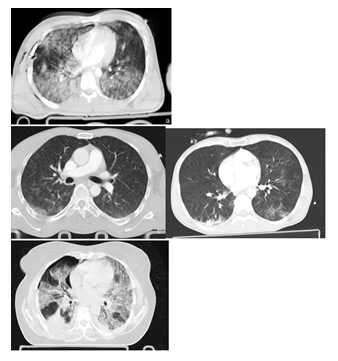
Figure 2: Axial slices of Chest CT scans with lung window a) a 30 y/o male with MVA in pre-COVID-19 era and multiple peripheral and central irregular and round GGO and b) a 24 y/o male with MVA and lung contusion also COVID-19. Initial CT scan showing multiple peripheral and central GGO. c) A 40 y/o male with MVA in pre-COVID-19 era and multiple diffuse irregular GGO and d) a 58 y/o female came to ER with CTO and COVID-19 pandemic and in initial CT scan showing multiple diffuse irregular GGO.
|
Lung Opacities |
CC group patients |
CO group patinets |
||||||
|
Shape |
Irregular |
Round |
Irregular and round |
Irregular |
Round |
Irregular and round |
P- Value |
|
|
GGOs |
2 (22%) |
3(33%) |
3 (33%) |
6 (37.5%) |
6 (37.5%) |
4 (25%) |
0.448 |
|
|
Consolidations |
4(45%) |
2(22%) |
3 (33%) |
10(62.5%) |
2 (12.5%) |
4 (25%) |
0.666 |
|
|
Location |
Peripheral |
Diffuse |
Peripheral |
Paraspinal |
Diffuse |
|||
|
GGOs |
1 (11%) |
7 (78%) |
9 (56%) |
0 (0%) |
7 (44%) |
0.034 |
||
|
Consolidations |
3 (33%) |
6 (67%) |
11 (69%) |
3 (19%) |
2 (12%) |
0.01 |
||
|
Subpleural sparing |
4 (44%) |
15 (93.8%) |
0.005 |
|||||
|
Pattern |
Multiple |
Single |
Multiple |
|||||
|
GGOs |
8 (89%) |
0 (0%) |
16 (100%) |
0.146 |
||||
|
consolidations |
9 (100%) |
0 (0%) |
15 (93.8%) |
0.339 |
||||
|
Spread |
Unilateral |
Bilateral |
Unilateral |
|||||
|
0 (0%) |
9 (100%) |
2 (12.5%) |
0.17 |
|||||
|
Crazy paving |
1 (11%) |
2 (12.5%) |
0.918 |
|||||
|
Atoll sign |
0 (0%) |
2 (12.5%) |
0.17 |
|||||
|
Reticular line |
4 (44%) |
13 (81.3%) |
0.06 |
|||||
|
Associated injuries |
||||||||
|
Rib fracture |
0 (0%) |
4 (25%) |
0.046 |
|||||
|
Pleural effusion |
0 (0%) |
3 (19%) |
0.088 |
|||||
|
Pneumothorax |
0 (0%) |
10 (63%) |
0.009 |
|||||
|
cavitation |
0 (0%) |
6 (37.5%) |
0.012 |
|||||
Table 2: Lung opacities and distributions
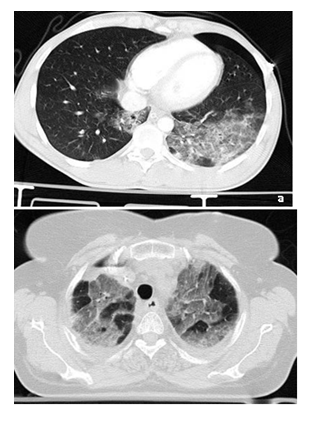
Figure 3: Axial slices of Chest CT scans at lung window of two patients with crazy paving appearance a) in a 28 y/o male with MVA in pre-COVID-19 era and b) in a 58 y/o female with CTO in a patient with COVID-19.
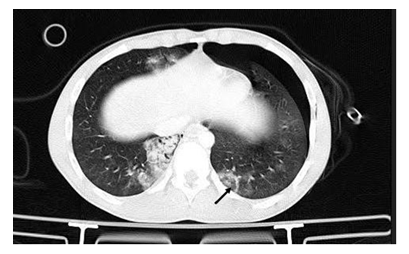
Figure 4: Axial slice of Chest CT scan at lung windows at level of the diaphragm in 17 y/o male from pre-COVID19 era with car turn-over and reversed halo sign (arrow) consisting of central GGO and peripheral consolidation involving more than 75% of the periphery of the lesion.
3.2 Distribution in lung parenchyma
The GGO locations were more likely to be diffusely distributed in CC patients with bilateral lung involvement in 78% of the CC group as opposed to 44% of the CO group (p= 0.034; Table 2). Consolidations were also more diffuse in the CC group (67%) comparing to the CO (12%) (p= 0.01). Peripheral distribution of GGOs were noted in only one out of nine CC patients and nine out of 16 cases in the CO group (p=0.034). Furthermore, the peripheral distribution of consolidations was recognized in three out of nine CC patients and 11 out of 16 Cases in the CO group (p=0.01). Sub pleural sparing was observed in 15 (93.8%) of CO and only four (44%) of the CC patients (p<0.005) (Figure 5).
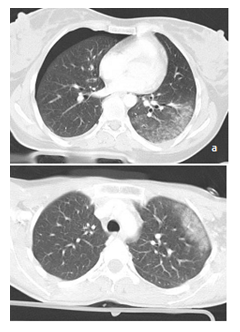
Figure 5: Axial slices of Chest CT scan at lung window in a) a 29 y/o female with CTO in pre- COVID19 era and b) a 26 y/o female with MVA and COVID-19, both showing peripheral ground glass opacity with sub pleural sparing.
3.3 Resolution of lung opacities
Out of the nine cases in CC group, two were deceased with significant increased pulmonary involvement in the follow up CT-scan (Figure 6c, d), five cases had positive findings more than ten days after hospital admission and in two cases, CT-scan findings were seen to be resolved up to ten days after hospitalization (Table 3). In the CO control group, ten cases showed CT-scan resolution in the follow up imaging during the period of five days from admission (Figure 6a, b). The CT resolution of areas of lung contusion occurred in the remaining cases up to ten days from admission. Comparison between these two groups was significant (p<0.001) (Figure 6). In six patients of the CO group, however, there were areas of laceration which took longer to resolve.
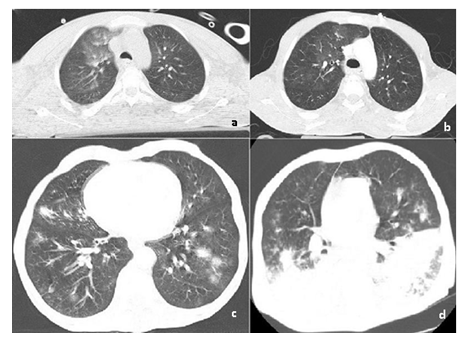
Figure 6: Axial Chest CT slices with lung window at presentation (a and c) and after 7 days (b and d) in two patients from pre-COVID19 era (32 yo male with MVA; a and b) and COVID19 and lung contusion (28 yo male, c and d). While the opacities have nearly completely resolved in the patient with contusion (a and b); in the patient with COVID-19 the progress of the chest CT opacities proceeded progression of the disease. Patient was deceased in day 17 of his hospital admission.
|
Less than 5 days |
5 to 10 days |
More than 10 days |
Deceased |
P-value |
|
|
CC group patients |
0 (0%) |
2 (22%) |
5 (56%) |
2(22%) |
0.001 |
|
CO group patients |
10 (62.5%) |
6 (37.5%) |
0 (0%) |
0 (0%) |
Table 3: Time of resolution of lung contusion
4. Discussion
COVID-19 is a viral disease with devastating consequences on public health and world economy. The virus can manifest clinically with a significant number of patients remaining asymptomatic. Many have reported incidental detection of COVID-19 in CT-scans taken for other causes. While RT-PCR is the gold standard for diagnosis, it is limited in sensitivity (<70%).[6,15-17] and availability. CT-scan is widely available but the features that are considered typical for COVID-19 are nonspecific. Features such as GGO and consolidation with peripheral distributions, round opacities, bilateral and multilobular involvement can be seen in many forms of pneumonia, both viral and bacterial, as well as noninfectious etiologies. Specifically, in lung contusions one of the most common findings are peripheral GGO.
In communities hit by the COVID-19 outbreak, hospitals have been struggling with resource allocation and bed management. In the absence of a fast and accurate diagnostic test allocating patients to COVID-19 and non-COVID-19 wards is a challenge. Considering all patients as positive for COVID-19 is not practically possible given the financial burden of airborne precautions. While under-diagnosis can harm the staff, over diagnosis can risk the patients by putting them in the potentially infectious department. We compared CT-scans in trauma patients with COVID-19 with patients with lung contusion in pre-COVID-19 era to evaluate the predictive value of features considered typical for COVID-19 in diagnosing COVID-19 in trauma patients.
Bilateral GGOs which are considered typical for COVID-19 are common in trauma too. Contusions are also commonly bilateral and usually peripheral in trauma [10].We found bilateral GGOs in all of our cases with both contusion and COVID-19and in 14 (87.5%) of our pre- COVID-19 lung contusion cases. On the other hand, diffuse GGO (seven, 78%) and consolidations (six, 67%) were more common in COVID-19 as opposed to patients with lung contusion (respectively seven, 44% and two, 12%).
We also found that the peripheral distribution considered a classic chest CT-scan finding for COVID-19, [18] is not a distinctive factor in patients with lung contusion who are also suspected of having COVID-19. Also while round GGOs are considered typical for COVID-19.[19,20] in this study the shape of opacities whether GGOs or consolidations, were not deemed different between the two groups (p=0.448 and p=0.666 for consolidations and GGOs respectively.
Crazy paving is the term used to describe coexistence of GGOs with inter- and intra-lobular septal thickening. This pattern has been described in many different disorders such as Acute Respiratory Distress Syndrome (ARDS) and pulmonary hemorrhage. In COVID-19 pneumonia the crazy paving appearance is seen usually late in the second week [18,21]. In our series, two of the pre-COVID-19 era patients with lung contusion carried this feature whereas in one of the lung contusion patients with COVID-19 this sign was observed (Figure 3). Reversed halo sign
i.e. atoll sign is considered a typical finding in organizing pneumonia. It consists of central GGO and peripheral consolidation. This finding was seen in two out of 16 of pre-COVID-19 trauma cases. While we are aware that this appearance is considered to be caused by organizing pneumonia, we believe that the random occurrence of GGO and consolidations can sometimes result in appearances resembling atoll sign. The reverse halo was however seen in none of the lung contusion cases with COVID-19. This is not unexpected considering the fact that Atoll sign is a rare sign seen in the late phases of the disease and unlikely to be seen in asymptomatic subjects [22,23].
The time course of the opacities was however distinctively different between the two groups. The opacities considered to be lung contusion were resolved almost completely in a period of five days to ten days from admission. However, patients with COVID-19 pneumonia seem to have prolonged period of resolution. In a study by Feng Pan et.al the uttermost severity of lung abnormalities is observed in ten days after admission.24 Given that the COVID-19 cases in this study were incidentally detected, we expect them to be either asymptomatic carriers or in the early stages of the disease. Taking more than ten days to resolve is however consistent with COVID-19, an in the absence of cavities indicating lacerations, can be considered a distinctive finding suggesting co-existing COVID-19 pneumonitis rather than simple contusions. Our study associated with limitations of small sample size and retrospective design
5. Conclusion
During the recent COVID-19 outbreak, lung contusion opacities in the chest CT-scan of traumatic patients need to be differentiated from pulmonary involvement by COVID-19 in the subclinical state. There is a great degree of overlap of the findings considered typical for COVID-19 with the findings previously described in lung contusion. When findings including peripherally located GGOs are encountered in patients with motor vehicle accidents, clinical findings and RT-PCR should be considered before making a hasty diagnosis of COVID-19. Admission in the so-called gray zones should be considered before labeling the patients as COVID-19.
Funding
authors report no conflict of funding sources
Acknowledgements
This article edited by native English editor (Arya Zamiri and Mohammad Javad Zamiri). It should be noted that an earlier version of this manuscript has been submitted to https://www.researchsquare.com/article/rs-29806/v1 as a preprint.
Authors' contributions
All the authors have contributed in conceptualization of the study. SS, FZ have acquired the cases and data and methodology. SHJ, FZ and NS have read and interpret the images. SS and NS have done the statistical analysis and article draft. All the authors have contributed in final editing and critical reviewing and approval of manuscript to be published.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Shiraz University of Medial Sciences ethics committee. Reference number of the study is IR.SUMS.REC.1399.321.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study
Competing interests
The authors declare that they have no competing interests
References
- Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill 25 (2020): 2000058.
- Tuite AR, Bogoch II, Sherbo R, Watts A, Fisman D, et al. Estimation of coronavirus disease 2019 (COVID-19) burden and potential for international dissemination of infection from Iran. Ann Intern Med 172 (2020): 699-701.
- Yadollahi M, Gholamzadeh S. Five-year forecasting deaths caused by traffic accidents in Fars province of Iran. Bull Emerg Trauma 7 (2019):373-380.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (2020): 497-506.
- Gostic K, Gomez AC, Mummah RO, Kucharski AJ, Lloyd-Smith JO. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife 9 (2020): e55570.
- Yang Y, Yang M, Yuan J, Wang F, Wang Z, et al. Laboratory diagnosis and monitoring the viral shedding of SARS-CoV-2 infection. Innovation (N Y) 1 (2020):100061.
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. Am J Roentgenol 215 (2020): 87-93.
- Zhu Y, Liu Y-L, Li Z-P, Kuang J-Y, Li X-M, et al. Clinical and CT imaging features of 2019 novel coronavirus disease (COVID-19). J Infect 81 (2020): 147-178.
- Wei J, Xu H, Xiong J, Shen Q, Fan B, et al. 2019 Novel coronavirus (COVID- 19) pneumonia: Serial Computed Tomography Findings. Korean J Radiol. 21 (2020): 501-504.
- Kaewlai R, Avery LL, Asrani AV, Novelline RA. Multidetector CT of blunt thoracic trauma. Radiographics 28 (2008): 1555-1570.
- Reddy NB, Hanumantha PM, Reddy NN, Reddy CS. An epidemiological study on pattern of thoraco-abdominal injuries sustained in fatal road traffic accidents of Bangalore: Autopsy-based study. J Emerg Trauma Shock 7 (2014): 116-120.
- Oikonomou A, Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging 2011;2:281-95.
- Mirka H, Ferda J, Baxa J. Multidetector computed tomography of chest trauma: indications, technique and interpretation. Insights Imaging 3 (2012): 433-449.
- Shi H, Han X, Jiang N, Cao Y, Alwalid O, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 20 (2020); 425-434.
- Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill 25 (2020): 2000045.
- Ai T, Yang Z, Hou H, Zhan C, Chen C, et al. Correlation of chest CT and RT- PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 296 (2020); E32-E40.
- Fang Y, Zhang H, Xie J, Lin M, Ying L, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 296 (2020): E115-E117.
- Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology 296 (2020): E46-E54.
- Inui S, Fujikawa A, Jitsu M, Kunishima N, Watanabe S, et al. Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiol Cardiothorac Imaging 2 (2020): e200110.
- Fang Y, Zhang H, Xu Y, Xie J, Pang P, et al. CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 10(2020): 200280.
- Rossi SE, Erasmus JJ, Volpacchio M, Franquet T, Castiglioni T, et al. “Crazy-paving” pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics 23 (2003): 1509-1519.
- Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology 7 (2020):200463.
- Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol 21 (2020): 494-500.
- Pan F, Ye T, Sun P, Gui S, Liang B, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 19(2020):200370.
- Donnelly LF, Klosterman LA. Subpleural sparing: a CT finding of lung contusion in children. Radiology 204 (1997): 385-387.
- Ajlan AM, Ahyad RA, Jamjoom LG, Alharthy A, Madani TA. Middle East respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings. Am J Roentgenol 203 (2014):782-787.
- Chung M, Bernheim A, Mei X, Zhang N, Huang M, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 295 (2020): 202-207.
- Ng M-Y, Lee EY, Yang J, Yang F, Li X, et al. Imaging profile of the COVID- 19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaginh 2 (2020): e200034.
