Characteristics Associated with Success for Opioid Use Disorder Treatment in Court-involved Patients
Article Information
Li Li*, Bianca M Bryant, Christina Cenczyk, Brian Gawronski
Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, Birmingham, AL, USA
*Corresponding Author: Li Li, MD, Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, 1720 University Blvd., Birmingham, AL, 35294, USA
Received: 08 November 2020; Accepted: 16 November 2020; Published: 08 December 2020
Citation: Li Li, Bianca M Bryant, Christina Cenczyk, Brian Gawronski. Characteristics Associated with Success for Opioid Use Disorder Treatment in Court-involved Patients. Archives of Clinical and Biomedical Research 4 (2020): 749-759.
Share at FacebookAbstract
Objectives: While the Food and Drug Administration (FDA) have approved medications for opioid use disorder (MOUD), they are underutilized with patients despite established effectiveness. The aim of the present study was to characterize the effectiveness of MOUD in a community-based drug court-involved population.
Methods: This is a two-year retrospective study of electronic health records data of patients at a community-based substance use treatment program who were involved in drug court and treated with MOUD from March 2018 to February 2020. Patients treated with buprenorphine products and extended-release injectable naltrexone were eligible to be in the study. Electronic medical records were used to collect patients’ demographics, clinical characteristics, and the results of urine drug screening throughout their treatment course.
Results: Of the 125 patients enrolled in the study, 100 (80%) of the patients were on buprenorphine products. Females had a greater retention rate with the medication management and a higher rate of sobriety measured by negative urine tests. Gender, treatment duration, and number of clinic visits were positively associated with sobriety and a better outcome. The number of clinic visits was the best predictor of sobriety as measured by negative urine tests.
Conclusions: MOUD is effective in patients involved in the drug court, although buprenorphine products are more acceptable than extended-release injectable naltrexone. Females seem to do better in terms of the retention and sobriety rates. The number of clinic visits and treatment duration are associated with better treatment outcomes.
Keywords
Medications for opioid use disorder; Buprenorphine; Court-involved; Number of clinic visits; Urine drug screening
Medications for opioid use disorder articles; Buprenorphine articles; Court-involved articles; Number of clinic visits articles; Urine drug screening articles
Article Details
1. Introduction
Opioid use disorder (OUD) has become an increasingly public health concern in the last few decades. The number of people in the U.S. who used heroin increased from 214,000 in 2002 to 359,000 in 2010 [1]. Prescription opioid use has also escalated. It is estimated that over 2.1 million people in the U.S. are addicted to heroin, prescription opioid, and/or illicitly manufactured fentanyl and its analogues [2]. Prescription and non-prescription opioids are among the most commonly misused drugs in the U. S. with 47,600 opioid overdose death in 2017 [3]. In addition to opioid overdose deaths, OUD is also associated with morbidity and mortality from HIV, hepatitis, criminal behavior, arrest, and incarceration [4-6].
Drug courts, specialized court docket programs that target criminal defendants and offenders, et al, have become increasingly popular in the U.S. as a means of diverting non-violent drug offenders away from jails and prisons into more treatment-oriented settings [7-10]. Available evidence suggests that drug courts contribute to reduced crime and less illicit drug use. Benefits of drug courts also include increased accountability and supervision to aid in sobriety, a decrease in drug usage and recidivism, and demonstrated cost effectiveness due to the allocation of funds toward treatment rather than a correctional facility [11]. Similar to the previously described upward trends, the number of people in drug courts with opioid misuse has also increased over the past decade. In a 2014 national survey, adults under drug court supervision ranked opioids as the primary substance of misuse [12].
Pharmacotherapy, which is therapy using medications, is one treatment option for individuals with OUD. There are three medications approved by FDA to treat OUD, including methadone, buprenorphine and naltrexone. Increased amount of evidence supports that medications for OUD (MOUD) are effective in reducing heroin and prescription opioid misuse as well as criminal behavior, human immunodeficiency virus risk behaviors, and overdose deaths associated with opioid misuse [13-15]. These medications are also cost-effective [16]. For justice-involved adults, MOUD has been shown to reduce opioid use, incarceration, heroin use, relapse to opioid use, and illegal activity [17-19]. However, a national study showed that approximately half of drug courts indeed prohibited the use of MOUD [20, 21]. It is reported that MOUD is made available by 38-56% of drug courts. Thus, MOUD is significantly underutilized in population involved in drug courts. Therefore, it is critical to understand the barriers for underutilizing MOUD in drug court population. In other words, what will contribute to the success of MOUD in this population? Additionally, there is limited data on patients’ characteristics, predictive factors, and treatment outcomes for MOUD in drug court population.
The Beacon Recovery Program, established more than 30 years ago, is outpatient-based and also a drug court designated program for patients with substance use disorder, including OUD. However, MOUD was not part of the treatment until March of 2018. Since March of 2018, the clinic for MOUD and primary psychiatric illness has started to serve the patients at Beacon Recovery Program. Thus, we conducted a two-year retrospective study using electronic medical records for drug court-involved patients in the program to assess: 1) the efficacy of MOUD in this particular population; 2) characteristics and predictive factors for successful treatment outcomes regarding MOUD; and 3) the comorbidity of primary psychiatric illness in this particular population.
2. Methods
2.1 Participants
We performed a 24-month retrospective study using deidentified electronic medical record data on 125 patients involved in courts who received care through the Beacon Recovery Program from March 2018 to February 2020. When the patients were enrolled, they had the opportunities to be followed for up to 12 months by the program. Patients were also required to participate in psychosocial and behavioral therapies as ordered by the courts and referred to the Beacon clinic at the same time. All the enrolled 125 patients completed their service in the program by February 2020, and any active patients with the program by March 1st 2020 were excluded from data collection. Among these 125 patients, each patient was either treated with buprenorphine products or extended-release injectable naltrexone. The project was approved by the Institutional Review Board at the University of Alabama at Birmingham and was conducted in accordance with the Helsinki Declaration of 1975. Diagnosis for OUD and primary psychiatric illness were made by the clinicians using the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, criteria. The co-occurring OUD and psychiatric illness, a phenomenon also referred to as comorbidity or dual diagnosis, was observed in the present study [22]. The patients were assessed by physicians and treated with medications at no cost. Urine drug screenings (UDS) were conducted randomly and/or on the day of their clinic visits. The electronic medical records were reviewed for their demographics, addiction history, smoking status, adverse trauma exposures, and physical health. Success for MOUD in this study is defined as negative UDS tests and retention in the treatment.
2.2 Statistical analysis
All analyses were conducted using the Statistical Package for the Social Sciences, version 26 (Chicago, IL), and p value was set at <0.05 as significant. Continuous data are presented as means (±standard deviation). Differences between the two groups in variables of interest were compared using Chi-square test for categorical data, including gender, race, education levels, and employment, and using independent T-test for continuous data, including age and buprenorphine product dosage. Analysis was performed to determine correlation between engagement in treatment (treatment duration and number of clinic visits) and numbers of negative UDS results during the treatment. Stepwise linear regression was used to supplement correlational evidence to further evaluate factors that predict negative UDS results. Multiple factors, including age, gender, race, length of drug misuse, employment, education, treatment duration, and the number of clinic visits were entered into the model. Criteria were 0.05 for entry and 0.1 for removal.
3. Results
3.1 Participant Characteristics
As shown in Table 1, the total sample of the study consisted of 37 (30%) African Americans and 88 (70%) Whites (self-identified as non-Latino or non-Hispanic ethnicity) individuals. Women comprised 51% of the sample. The average age was 36 years. There were no significant differences for race, education, smoking and employment statuses, and years for illicit drug use between male and female patients. Of the male and female patients, approximately 50% of them had a dual diagnosis, including anxiety and depression, and 84% of patients received medications for their primary psychiatric disorders. Both male and female patients reported a history of trauma. Female patients tended to have a higher percentage for a history of trauma, but not significantly.
A majority of female and male patients were taking buprenorphine products, including buprenorphine and buprenorphine/naloxone, and a few were on extended-release injectable naltrexone (Table 2). Effective dosage of buprenorphine was between 10-16 mg, sublingual, daily. Patients with MOUD were usually seen weekly in the first 2 weeks, then bi-weekly for 2 times, and then monthly or bi-monthly afterwards when they were stable with MOUD. However, patients were provided with flexibility for clinic visits as often as indicated. The average numbers of clinic visits were 5.3 and 7.6 for males and females, respectively (p<0.01). Of the male participants, 33 had fewer than 5 clinic visits. However, of the female participants, only 21 had been seen fewer than 5 times in the clinic before they were lost to follow up, and more than 15 females remained in the clinic for 12 months throughout the course of recovery treatment program (Table 2).
3.2 Correlational analysis
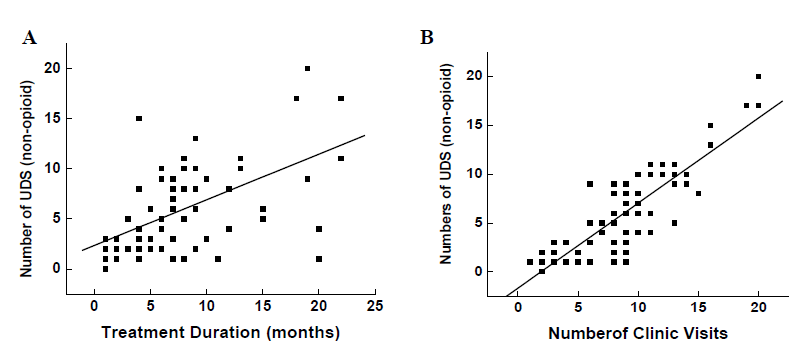
UDS tests were completed randomly or on the day of their clinic visit in each patient. Correlational analysis indicated that negative urine tests associated with treatment duration (r=0.57, p<0.000), and the number of clinic visits (r=0.76, p<0.000) in patients (Figure 1A and B).
3.3 Predictive model
The results of the multivariate analyses predicting the sobriety as measured by negative urine tests as a function of gender, race, treatment duration, number of clinic visits, and primary psychiatric illness can be seen in Table 3. For both men and women, negative urine tests were best predicted by the number of clinic visits.
Table 1: Participants Characteristics.
|
Characteristics |
Total |
Males |
Females |
P values |
|
N |
125 |
61 |
64 |
|
|
Ages (years), mean (SD) |
- |
36.6 ± 9 |
36.2 ± 9 |
- |
|
Race, White/Black, N |
88/37 |
43/18 |
45/19 |
0.51 |
|
<HS education, N |
68 |
35 |
33 |
0.52 |
|
Employment, N |
21 |
18 |
13 |
0.29 |
|
Current smoker, N |
95 |
49 |
46 |
0.49 |
|
Years of illicit drug use, N |
||||
|
1-5 years |
26 |
11 |
15 |
0.89 |
|
>5-10 years |
30 |
12 |
18 |
0.82 |
|
>10 years |
69 |
38 |
31 |
0.51 |
|
History of trauma, N |
34 |
13 |
21 |
0.055 |
Notes: <HS, less than a high school education
Table 2: Comparisons between male and female patients.
|
Comparisons |
Males |
Females |
P values |
|
Buprenorphine, N |
48 |
52 |
|
|
Buprenorphine dosage (mg), mean (SD) |
14.8 ± 6.8 |
12.3 ± 5.2 |
0.046 |
|
Extended-release naltrexone, N |
5 |
4 |
- |
|
Dual-diagnosis, N (%) |
29 (48%) |
34 (52%) |
- |
|
Number of clinic visits, N |
|||
|
1-5 times |
35 |
23 |
0.025 |
|
>5-10 times |
18 |
25 |
0.024 |
|
>10 times |
8 |
16 |
0.009 |
|
Treatment duration |
|||
|
1-3 months |
31 |
24 |
0.080 |
|
>3-6 months |
12 |
12 |
0.568 |
|
>6 months |
18 |
28 |
0.002 |
Table 3: Stepwise linear regression analysis predicting negative UDS results.
|
Significant Predictors |
R2 |
B |
P |
|
|
Male (n=61) |
Number of clinic visits |
0.71 |
4.17 |
0.000 |
|
Female (n=64) |
Number of clinic visits |
0.58 |
5.43 |
0.000 |
Notes: Independent variables included age (years), race (0=Caucasian, 1=African American), dual diagnosis (0=no, 1=yes), employment, education, smoking, treatment duration, number of clinic visits, years of illicit drug abuse, buprenorphine dosage (mg), history of trauma; Abbreviations: UDS, urine drug screening
4. Discussion
Our findings in a drug court-involved population clearly indicate that MOUD is an effective approach to treat patients with OUD in terms of negative UDS tests and retention in the treatment. It was previously thought women made up a smaller percentage of patients engaged in criminal justice MOUD [23]. In contrast, we had nearly 50% female patients receiving MOUD. In the present study, more Caucasians were seen in our clinic for MOUD. Our observation is consistent with previous reports [7]. Gender differences were observed between patients receiving MOUD. Retention rate is lower in males
than in females because males dropped out or were lost to follow up at higher rates than females. Sobriety is higher in females than in males although females are on lower dosage of buprenorphine products. Male patients have fewer negative urine tests than females because they tend to drop out of treatment earlier. Thus, it can be inferred from our data that more office visits lead to a better retention rate and a longer duration of sobriety. There is a higher rate of dual diagnosis in the criminal justice system than previously thought [24], however, this does not appear to be gender-specific in our study. Our findings indicate that treatment duration is associated with favorable outcomes, and the number of office visits is the best predictor for an individual’s sobriety measured by negative urine tests.
Despite the efficacy of MOUD, fewer than half of drug courts offer MOUD to their patients diagnosed with OUD [20]. This can partly be attributed to barriers such as access to treatment, negative attitudes toward opioid agonists as a form of treatment, and the stigma associated with MOUD
This stigma is pervasive in the community and is even held by drug treatment professionals and drug users [25-27]. The stigma derives from concerns associated with diversion, beliefs that methadone generates an array of unwanted side effects, and opinions that MOUD use prevents patients from achieving full abstinence (i.e., keeps them addicted to another opioid). Many of these beliefs are based on a misunderstanding of how methadone functions or a philosophical bias against maintenance medication in favor of interventions that do not use medications [28-30]. Research has indicated that bias or misinformation about benefits and risks associated with methadone results in poorer treatment outcomes
Bias has played a significant role in limiting expansion of methadone treatment and has led to counter-therapeutic rules on methadone treatment such as imposing a ceiling dose or limiting duration of treatment [31-34].
The extent to which negative attitudes toward methadone extend to buprenorphine treatment is currently unclear. Despite the efficacy of buprenorphine, several stigmas are associated with using buprenorphine as a treatment option. Many providers see buprenorphine as a scapegoat to continue drug use [35]. They also fear that patients
prescribed buprenorphine will either use it to get high or sell the drug for profit [35]. However, our results support the use of buprenorphine products in this population, especially with regards to community substance use treatment engagement and discontinuation of opioids use. The current study provided further evidence that buprenorphine products are effective to treat the patients with OUD in court-involved population. In addition, our data indicated that negative urine tests are associated with both treatment duration and the number of clinic visits. Consistent with literature, our predictive model suggests that adherence with MOUD treatment, especially attending the appropriate number of clinic visits, is a predictor of sobriety as measured by negative urine tests [35, 36]. However, its relationship with both recidivism and initial criminal justice involvement warrants future examination before results can be generalized.
Mental illness and self-medication through substance use are two pathways to incarceration that are often mentioned in the literature [37, 38]. Literature has reported that about half the individuals diagnosed with substance use disorder have some type of concurrent mental illness. In our study, the prevalence of dual diagnosis is much higher (~50%) than previously thought, which suggests a large need for dual care of mental health as well as substance use services [39, 40]. Individuals with a dual diagnosis suffering from both psychiatric disorders and substance use are often not treated simultaneously. Treatment of dual diagnosis of both OUD and primary psychiatric illness should be addressed accordingly. Treatment with or without medication alongside some form of therapy, i.e. cognitive behavioral therapy or dialectical behavioral therapy, is warranted for those with dual diagnosis When treating both OUD and primary psychiatric illness, they should both be addressed rather than treating one or the other.
Although it is known that the engagement in treatment would lead to a favorable outcome, adherence has been an issue in substance use treatment. Several studies have shown that adolescents and young adults who participate in MOUD have a greater retention rate as opposed to those only receiving behavioral therapy to treat OUD [35, 42]. Identifying non-adherence in the initial stages of treatment helps to increase retention [36]. In the present study, female patients had better adherence than their male counterparts. Reasons could be their demanding roles in their family, their commitment to recovery, and their guilt over opioid misuse. Thus, our data provides some evidence that MOUD may have a different impact on women in the court-involved population compared to their male counterparts. Additionally, these findings warrant replication in a larger sample.
Results of this study should be considered in the light of its limitations. First, our findings are from a retrospective study at a single site, which might have a selection bias. Caution should be taken when generalizing our findings. Second, patients in the Beacon Recovery Program are required to attend psychosocial behavioral therapy, which was not included in the data analysis. Future studies should consider the impact of psychosocial therapy on the adherence for patients with MOUD. Third, our observation is consistent with other reports that buprenorphine products are more acceptable than extended-release injectable naltrexone, although both are effective in OUD treatment. Since the Beacon Recovery Program is an outpatient-based treatment program, patients experienced difficult going through 5-14 days of opioid-free time before extended-release injectable naltrexone could be administered. In our study, the administrated numbers of naltrexone ranged from 1-5 among 9 patients. Thus, strategic plans may need to be established to facilitate this opioid-free period for extended-release injectable naltrexone initiation and maintenance. Fourth, data on marital status and number of children in each patient was incomplete, and the program did not collect data on recidivism. Thus, these important variables will be included in future studies. Finally, our study focused exclusively on adults although the Beacon Recovery Program serves adolescents aged 13-18 years. Although buprenorphine products are approved for use in patients with OUD older than 16 years, little is known about barriers to MOUD in this young group in court-involved population. Therefore, more studies are warranted to understand this young population.
5. Conclusions
In summary, our findings provide further solid evidence that MOUD is an effective approach for court-involved patients, although gender differences were observed in terms of retention rate in the treatment and sobriety rate measured by negative urine tests. Our findings also highlight the importance of adherence with treatment, i.e., the number of clinic visits, for a better outcome.
Acknowledgments
We are grateful to the patients for their willingness to be served in the clinic.
Author Contributions
conceptualized and designed the study, supervised the study, performed statistical analysis, wrote and edited the manuscript. BMB wrote the manuscript and collected the data. CC collected the data and edited the manuscript. BG collected the data and edited the manuscript. All authors approved the final version.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Babor TF, Del Boca F, Bray JW. Screening, Brief Intervention and Referral to Treatment: implications of SAMHSA's SBIRT initiative for substance abuse policy and practice. Addiction 112 (2017): 110-117.
- Center for Behavioral Health Statistics and Quality (CBHSQ). 2017 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration (2018).
- Scholl L, Seth P, Kariisa M, et al. Drug and Opioid-Involved Overdose Deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep 67 (2018): 1419-1427.
- Joseph H. The criminal justice system and opiate addiction: a historical perspective. NIDA Res Monogr 86 (1988): 106-125.
- Mathers BM, Degenhardt L, Ali H. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet 375 (2010): 1014-1028.
- Nelson PK, Mathers BM, Cowie B, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet 378 (2011): 571-583.
- Brown RT. Systematic review of the impact of adult drug-treatment courts. Transl Res 155 (2010): 263-274.
- Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. Jama 301 (2009): 183-190.
- Kushel MB, Hahn JA, Evans JL, et al. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health 95 (2005): 1747-1752.
- Marlowe DB. Integrating substance abuse treatment and criminal justice supervision. Sci Pract Perspect 2 (2003): 4-14.
- Benefits of Drug Court. (2020). https://www.sanmateocourt.org/court_divisi ons/criminal/drug_court/benefits.php
- Marlowe DB, Hardin CD, & Fox CL (2016). Painting the current picture: A national report on drug courts and other problem solving courts in the United States Alexandria, VA: National Drug Court Institute Retrieved from http://www.ndcrc.org/sites/default/les/pcp_n al_version.pdf
- Nunn A, Zaller N, Dickman S, et al. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend 105 (2009): 83-88.
- Rich JD, Boutwell AE, Shield DC, et al. Attitudes and practices regarding the use of methadone in US state and federal prisons. J Urban Health 82 (2005): 411-419.
- Zaller ND, Yokell MA, Nayak SM, et al. Syringe acquisition experiences and attitudes among injection drug users undergoing short-term opioid detoxification in Massachusetts and Rhode Island. J Urban Health 89 (2012): 659-670.
- Barnett PG. Comparison of costs and utilization among buprenorphine and methadone patients. Addiction 104 (2009): 982-992.
- Dolan KA, Shearer J, White B, et al. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, re-incarceration and hepatitis C infection. Addiction 100 (2005): 820-828.
- Kelly SM, O'grady KE, Jaffe JH, et al. Improvements in outcomes in methadone patients on probation/parole regardless of counseling early in treatment. J Addict Med 7 (2013): 133-138.
- Schwartz RP, Mitchell MM, O'Grady KE, et al. Pharmacotherapy for opioid addiction in community corrections. Int Rev Psychiatry 30 (2018): 117-135.
- Matusow H, Dickman SL, Rich JD, et al. Medication assisted treatment in US drug courts: results from a nationwide survey of availability, barriers and attitudes. J Subst Abuse Treat 44 (2013): 473-480.
- Behind Bars II Substance Abuse and America’s Prison Population. (2010). https://www.centeronaddiction.org/addiction-research/reports/behind-bars-ii-substance-abuse-and-america’s-prison-population
- Drake RE, Mueser KT, Brunette MF. Management of persons with co-occurring severe mental illness and substance use disorder: program implications. World Psychiatry 6 (2007): 131-136.
- Drug Courts: Gender Differences and Their Implications for Treatment Strategies. (2002).
- Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry 56 (2004): 730-737.
- Forman RF, Bovasso G, Woody G. Staff beliefs about addiction treatment. J Subst Abuse Treat 21 (2001): 1-9.
- Kang SY, Magura S, Nwakeze P, et Counselor attitudes in methadone maintenance. Journal of Maintenance in the Addictions 1 (1997): 41-58.
- Rosenblum A, Magura S, Joseph H. Ambivalence toward methadone treatment among intravenous drug users. J Psychoactive Drugs 23 (1991): 21-27.
- Gerra G, Maremmani I, Capovani B, et al. Long-acting opioid-agonists in the treatment of heroin addiction: why should we call them "substitution"? Subst Use Misuse 44 (2009): 663-671.
- Kleber HD. Pharmacologic treatments for opioid dependence: detoxification and maintenance options. Dialogues Clin Neurosci 9 (2007): 455-470.
- White W. Philadelphia: Department of Behavioral Health and Mental Retardation Services; Long-term strategies to reduce the stigma attached to addiction, treatment, and recovery within the City of Philadelphia (with particular reference to medication-assisted treatment/recovery) (2009).
- D'Aunno T and Pollack HA. Changes in methadone treatment practices: results from a national panel study, 1988-2000. Jama 288 (2002): 850-856.
- Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med 67 (2000): 347-364.
- Magura S and Rosenblum A. Leaving methadone treatment: lessons learned, lessons forgotten, lessons ignored. Mt Sinai J Med 68 (2001): 62-74.
- Velander JR. Suboxone: Rationale, Science, Misconceptions. Ochsner J 18 (2018): 23-29.
- Warden D, Subramaniam GA, Carmody T, et al. Predictors of attrition with buprenorphine/naloxone treatment in opioid dependent youth. Addict Behav 37 (2012): 1046-1053.
- Connery HS. Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harv Rev Psychiatry 23 (2015): 63-75.
- Jones CM, Campopiano M, Baldwin G, et al. National and State Treatment Need and Capacity for Opioid Agonist Medication-Assisted Treatment. Am J Public Health 105 (2015): e55-63.
- DeHart DD. Pathways to prison: impact of victimization in the lives of incarcerated women. Violence Against Women 14 (2008): 1362-1381.
- Kelly TM and Daley DC. Integrated treatment of substance use and psychiatric disorders. Soc Work Public Health 28 (2013): 388-406.
- Ross S and Peselow Co-occurring psychoticandaddictivedisorders: neurobiology and diagnosis. Clin Neuropharmacol 35 (2012): 235-243.
- Baigent M. Managing patients with dual diagnosis in psychiatric practice. Curr Opin Psychiatry 25 (2012): 201-205.
- Hadland SE, Bagley SM, Rodean J, et al. Receipt of Timely Addiction Treatment and Association of Early Medication Treatment With Retention in Care Among Youths With Opioid Use Disorder. JAMA Pediatr 172 (2018): 1029-1037.