Challenges about Reorganizing a Hospital to Respond to the Covid-19 Outbreak: Experience from the University Hospital of Naples “Federico II”, Italy”
Article Information
Montella Emma1*, Frangiosa Alessandro1, Iodice Sabrina1, Bellopede Salvatore1, Trama Ugo2, Triassi Maria3
Affiliation:
1Department of Public Health, University of Naples “Federico II”, Italy
2Direzione Generale per la Tutela della Salute e il Coordinamento del Servizio Sanitario Regionale, Naples, Italy
3Department of Public Health, University of Naples “Federico II”, Naples; Interdepartmental Centre
for Research in Healthcare Management and Innovation in Healthcare (CIRMIS), University of Naples “Federico II”, Naples, Italy.
*Corresponding Author:Montella Emma, Department of Public Health, University of Naples “Federico II”, Edificio 12 D, Via Sergio Pansini, n 5, Napoli, 80131, Italy.
Received: March 16, 2023; Accepted: April 04, 2023; Published: April 13, 2023
Citation: Montella Emma, Frangiosa Alessandro, Iodice Sabrina, Bellopede Salvatore, Trama Ugo, Triassi Maria. Challenges about Reorganizing a Hospital to Respond to the Covid-19 Outbreak: Experience from the University Hospital of Naples “Federico II”, Italy”. Archives of Clinical and Medical Case Reports. 7 (2023): 148-154.
Share at FacebookAbstract
The 2020 pandemic has taken a toll on governments, hospitals and healthcare workers. The newly established Task Force of the University Hospital has sought to answer this huge challenge by applying a Hospital Incident Management System (HIMS). Given the lack of knowledge of this new pandemic, the System was created on the basis of previous organizational and structural models present in the literature and adapted to the Covid-19 pandemic. The response plan has included:
- The conversion or creation of cohorted areas for Covid-19 positive patients;
- The design of routes for pre-triage, diagnosis, and isolation of suspected and confirmed cases;
- The training of all the hospital staff to work with Covid-19 positive patients and the implementation of a health surveillance plan to protect workers for the prevention of clinical and non-clinical risk.
This system required a hospital multidisciplinary and interdepartmental collaboration, using the elements of Surge Capacity: (i) human resource management; (ii) supplies, equipment, logistics and replenishment mechanisms; (iii) specific skills for critical areas of care; (iv) overall management of hospital resources, such as the expansion of spaces and premises. Our goals were: the increase of hospital overload capacity to ensure a high level of care, the biocontainment of confirmed and suspected cases, to continue to provide safe critical care to non-Covid-19 patients and ensure a safe environment for both the healthcare operators involved and the patients. In this work we report our experience in the preparation of the hospital to the last health emergency.
Keywords
Covid-19; Decision Making; Hospital Incident Management; Pandemic; Risk Management; Surge Capacity
Covid-19 articles; Decision Making articles; Hospital Incident Management articles; Pandemic articles; Risk Management articles; Surge Capacity articles
Article Details
Case Report
The disease was first identified on December 31, 2019, by the health authorities of Wuhan, the capital of Hubei Province, China. The micro- organism strain, responsible for the pandemic, was identified in early January 2020 and its genome was released on January 10. On February 11, 2020, the World Health Organization (WHO) announced “Covid-19” as the name of the new coronavirus cause of the new disease called “Severe Acute Respiratory Syndrome Coronavirus 2” (SARS-CoV-2) [1]. The Covid-19 epidemic, in Italy, officially began on February 20, 2020, after the hospitalization of a patient in his 30s in the Intensive Care Unit (ICU) of Codogno Hospital (Lodi, Lombardy) who tested positive for SARS-CoV-2. During the following 24 hours, the number of reported positive cases increased to 36. In less than a week, the number of cases in Italy increased beyond expectations and positive patients were found, first in several neighbouring regions and autonomous provinces in Northern Italy, and later throughout all the Italian territory. In the Campania Region the first 3 cases were reported on February 27 [2]. In order to ensure healthcare and, considering the rapid spread of the disease, it was essential for all national care units to plan in advance the response, when the infection was yet to reach uncontrolled rates [3]. Therefore, a regional directive took effect on February 19, requiring hospitals to urgently prepare for a massive influx of Covid-19 positive patients. Hospitals were asked to convert intensive therapy units to cohorted units for critical Covid-19 positive patients and to create sub-intensive and medical units dedicated to subcritical positive patients. In response to this directive, on the very same day, the University Hospital “Federico II” established a Task Force composed by experts from different fields: (i) the General Director and the Administrative Director for the management of the political, legal, administrative and economic aspects; (ii) the Medical Officer Chief for Health Management; (iii) the Head of the Department of Public Health; (iv) the Risk Manager, to manage clinical and non- clinical risks; (v) the Head of the Department of Infectious Disease; (vi) the Head of Intensive Care Department; (vii) the Head of Department of Paediatric Infectious Disease;
(viii) the Nursing Director; (ix) the Director of Emergency
Assistance; (x) the Pharmacist and hospital pharmacologists, for the selection and supply of medicines; (xi) the Biomedical Engineer for the equipment management; (xii) the Structural Engineer for structural works. The objective of the Task Force was to develop governance guidelines to ensure emergency response by the hospital, to increase the hospital overload capacity to treat Covid-19 positive patients, to ensure a safe work environment both for patients and healthcare workers, to guarantee life-saving health cares for non-Covid patients. In order to contain both suspected and positive cases and to plan work activities, the Task Force had to rely on the instructions obtained from the scientific literature available at that time [4] on the consultation of experts and on the government regulation. Therefore, the Task Force designed a response plan called: Hospital Incident Management System (HIMS). The HIMS was organized into the following areas:
- Surge Capacity: the expansion of the hospital capacity through the reconversion of hospital spaces and the rational allocation of the available workforce;
- Risk Management for patients and staff: formation and training of the staff, intensive health surveillance program for workers;
- Guarantee of life-saving therapies: creation of pathways for patients, pre-triage, diagnosis, and isolation of both suspected and confirmed cases of Covid-19 [5].
The goal of our work is to describe our experience in preparing the hospital for the health emergency induced by Covid-19. In fact, we believe that sharing this work and the results may be useful to the scientific community.
Context Analysis
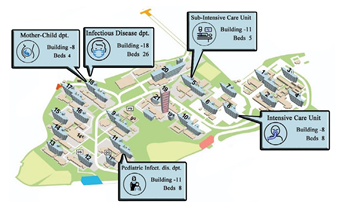
Our centre is a large multidisciplinary academic hospital in Southern Italy, equipped with 18 buildings (Figure 1). It has both surgical and medical expertise and it is the regional reference centre for rare adult and paediatric diseases, the reference centre for HIV treatment, the largest birth centre in Southern Italy with Gynaecological Emergency Aid, and offers surgical specialties and third level medical aid. It is, also, part of the network of kidney and marrow transplants. It has a total of 800 beds. Generally, includes an adult Intensive Care Unit with 8 beds and a Neonatal Intensive Care Unit with 20 beds, an adult Infectious Disease Department with 20 beds and a Paediatric Infectious Disease Department with 8 beds. In routine conditions, the Intensive Care bed use is always above 90%.
Surge Capacity
Intensive Care Unit - Building 8
The Intensive Care Unit (ICU) of the University Hospital is composed of an Airborne Infection Isolation Room (AIIR) equipped with negative pressure and limited access, dedicated to Covid-19 positive patients, with the first admission on the March 12, and 12 beds for Covid-19 negative patients. Until March 29, 2020, up to 12% of all positive cases required admission to ICU and the epidemiological data on the length of stay in ICU, of this kind of patients, was about 8 days [6]. For these reasons, on the same date, it was created a dedicated Covid-19 cohort, to use all available beds for Covid-19 patients. Our Covid-19 Intensive Care cohort was, in the emergency phase, one of the largest dedicated cohort intensive care units in Southern Italy. Covid-19 negative patients hospitalized
in ICU, were transferred to the Cardiac Surgery Intensive Care Unit (Building 2). One week after the conversion of the Intensive Care, on April 3, 2020, in order to reduce the effort in the intensive care unit, it followed the creation of a Sub-Intensive Care Unit (SICU) dedicated to patients with Covid-19 which did not require a third level of medical cares. The SICU was created by converting two operating theatres of the General Surgery Block (Building 5) whose activity was, at that time, suspended because of the pandemic. This choice was dictated by the structural configuration of the operating block that respected the national requirements: they allowed, indeed, to build exclusive and dedicated access for entry and exit to clean and dirty areas through filtering zones, for patients, operators, equipment, and personnel. The new SICU had 5 beds with intensive equipment: (i) nursing bed; (ii) multifunctional ICU ventilator; (iii) vital signs monitor; (iv) drug infusion system; (v) medical gas system;
(vi) anaesthesia machine. Each bed technology equipment, provided by the Italian Civil Protection Corp, didn't have appropriate supports and they were placed on surgical tables or laparoscopic racks which served as suitable alternatives. The ergonomic, in fact, was improper.
Department of Infectious Disease - Building 18
The Infectious Disease Department, is located on the third floor and has 14 beds, 10 of which are used for ordinary care and 4 assigned to isolate and treat HIV-infected patients. At the beginning of the emergency, on March 14, to respond immediately, the HIV patient area (4 beds) was transformed into a Covid-19 facility. Renovation works were carried out in 4 days and included the setup of a dressing and undressing area for each room. In addition, video monitoring systems were installed to limit operator’s access to patient rooms. The completion of the renovation made available, on March 25, an additional 4 beds with the same covid19 dedicated bed characteristics, for a total of 8 beds, 4 of which assigned to Covid-19 obstetric patients. On March 29, the entire Department of Infectious Disease became a Covid-19 cohort with 14 beds. On April 2, the building was entirely renovated and dedicated to Covid-19 positive patients with a total number of 26 beds.
Paediatric Infectious Diseases - Building 11
Children account for about 1-5% of diagnosed cases of Covid-19 [7]. In most cases, Covid-19 occurs in children asymptomatically or with mild symptoms. However, up to 6.7% of these cases may be serious. Patients younger than 1 year and patients with comorbidities suffer a more severe form of the disease [8]. At the time, the epidemiological contribution of children to disease transmission and drug therapy was not precisely defined. The University Hospital Paediatric Infectious Disease Centre (located on the 2nd floor of Building 11) was identified as the Covid-19 Paediatric Centre and Reference Hub for the Southern Italy. The entire unit was dedicated to patients with Covid-19, without the need of structural adjustments. Non-Covid-19 patients were moved to another floor of the same building that was already entirely dedicated to Paediatric Care.
Mother-Child Department - Building 9
The Mother-Child Department of the University Hospital attends to 2600 births every year. Therefore, it was designated as the Covid-19 Mother-Child Hub for the entirety of Southern Italy [9]. The dedicated safety paths required the creation of new spaces to ensure compliance with the containment measures [10]. Two triage tents were set up by the Italian Civil Protection, using adjacent flat spaces in front of the ward block. The tent 1 was dedicated to the access of pregnant patients with Covid-19, while the tent 2 to all other patients. Concerning Covid-19 positive pregnant patients, medical care was provided immediately in tent 1, suitably set up with: (i) gynaecological bed (ii) gynaecological care cart (iii) FHR detector (iv) amnioscope
(v) surgical lamp. Patients with Covid-19 who require obstetric-gynaecological surgical care, after the triage in the tent, were directed to a dedicated operating room, obtained from the remodelling of the Orthopaedic Surgery Block (Building 12), consisting of two rooms. The first room was dedicated to Covid-19 obstetric surgery and was fully equipped, according to national legislation. The structural and technological equipment allowed to face any type of obstetric-gynaecological surgery. The patient, therefore, after natural birth or caesarean delivery, was transferred to the Infectious Disease Department (Building 18) dedicated to patients with Covid-19 and assisted by gynaecological staff. The second operating room was converted into a nursery, adequately equipped, where the new-borns, born from an infected mother, were assisted.
Diagnostic Imaging – Building 16
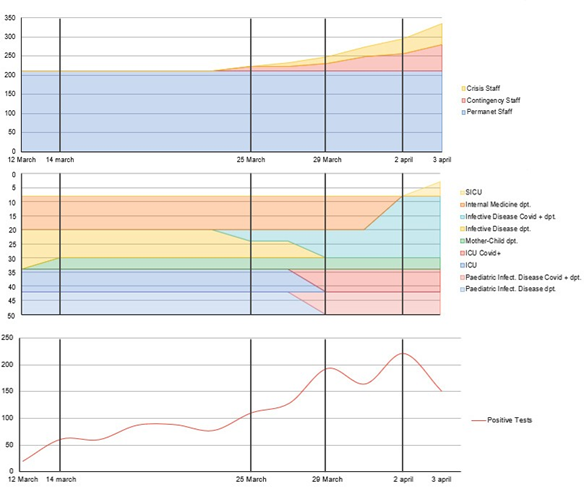
At the time the diagnosis of Covid-19 was based on the patient's medical history, clinical manifestations, imaging characteristics and laboratory tests. In particular, Computed Tomography (CT) of the chest played an important role in the initial diagnosis of SARS-CoV-2 pneumonia [11]. In the University Hospital, diagnostic imaging is generally performed in two different buildings (Buildings 10 and 16). At that time, the Building 16 was dedicated to Covid-19 positive patients, and the Building 10 was used for all other patients. Above mentioned bed changes are summarized in Figure 2.
Internal Transportation System
An ambulance, with a bio-containment stretcher and dedicated equipment, was designed within the vehicle fleet. Patients with Covid-19 were transferred from one building to another by this dedicated ambulance, through internal and one-way routes, identified with road signs.
Workforce
Surge Capacity includes the necessity to rationally distribute the available workforce and integrate support personnel. The Task Force of the University Hospital has included in the structure of the HIMS: (i) reassessment of the risk model for operators assigned to work units different from the previous; (ii) recruitment of qualified personnel;
(iii) redeployment of Covid-19 personnel: from routine activities to urgent activities related to Covid-19. For all those who worked with Covid-19 positive patients, the work shift system has been modified, particularly for intensive and sub-intensive cohorted therapy units, considering the inconvenience of working with PPE, including overheating and the impossibility to access food, water, and sanitary services, it was developed a system of 4 shifts per day (every 6 hours) with a one to two nurse-patient ratio and one to five medical doctor-patient ratio. The pool of doctors and nurses experts in intensive care has been divided between Intensive Care and SICU; the work shift of doctors and nurses were reinforced by the surgical operating theatre staff made available due to the drastic reduction of elective surgical activity caused by the pandemic. The doctors and nurses experts in infectious diseases were divided between the Infectious Disease Department and the Mother-Child area and the shift have been reinforced with staff from other areas. In total, the reinforcement nursing staff was made up of 61% of staff from other areas and 39% of newly recruited personnel, while the medical staff was made up of 52% of staff from other areas and 48% of new hired staff. This organization (Table 1) made it possible to respond with three phases: (i) Permanent Personnel: qualified healthcare personnel already available in the departments involved in the emergency (Intensive Care Unit, Department of Infectious Diseases, Department of Paediatric Infectious Diseases, Department of Gynaecology and Neonatal Intensive Care Units); (ii) Contingency Personnel: healthcare personnel newly hired and qualified to work in the Covid departments; (iii) Crisis Personnel: healthcare personnel normally performing activities other than those of emergency [12].
Risk Management for Healthcare Staff
Considering that the development of the vaccine and the research on effective therapeutic protocols were still ongoing, the pressure on healthcare personnel kept intensifying in 2 forms of risk: the clinical risk, caused by SARS-CoV-2 and related secondary medical complications, and non-clinical risk, determined when carrying out work activity [14].
Clinical Risk: the safety of healthcare workers is essential to provide the best possible services to infected people. Healthcare workers were at high risk of contracting the infection [15]: in Italy they represented, at that time, 10% of the total cases of Covid-19 [16]. To protect healthcare workers during Covid-19 patient caring, they had to wear medical masks, gowns, gloves, and eye protections with goggles or face shields [17]. For aerosol generating procedures (tracheal intubation), masks had to be N95 or FFP2 and gowns or aprons should be liquid resistant [6,18]. The risk of infection for healthcare workers was also determined by the dressing and undressing procedures through self-contamination. Training on the specific steps of using and removing PPE and correct hands cleaning was essential [15]. Therefore, the University Hospital Task Force, organized the February 20, before the Covid-19 outbreak in Campania Region, a training event developed for all healthcare personnel, to ensure training on the correct behaviours to adopt regarding the use of PPE, dressing and undressing procedures (Table 2), waste disposal and sanification of the environments. The above procedures were easily accessible online by healthcare professionals. The strategies adopted to optimize the use of PPE, in anticipation of its global shortage, have been as follows: (i) Using physical barriers to reduce exposure to the Covid-19 virus, such as glass or plastic windows whenever possible; (ii) Use of telemedicine (telephone triage) for early identification of suspected Covid-19 cases; (iii) Limitation of the number of healthcare professionals in patient’s rooms (including the help of video surveillance). Worker safety was also guaranteed through a risk-specific health surveillance protocol. This included the re-evaluation of the risk for operators assigned to work in departments different from the previous ones, regular visits, serological tests, and nasopharyngeal swabs for all suspected operators of Covid-19 infection [19].
Non-Clinical Risk: The Covid-19 pandemic risks placed healthcare professionals around the world under extreme stress, having to make difficult decisions and work under an higher pressure. In the first phase of the Covid-19 pandemic process, the uncertainty staff perceived about patient health risked compromising the emergency plan. Therefore, on February 23, when there were still no cases of illness in Campania Region, the Task Force organized an educational event, which was shared through an information campaign curated by the University Hospital Press Office. The event included a plenary session and the distribution of information material (leaflets) and posted in the crowded areas of the hospital. Subsequently, during the emergency, they have been guaranteed direct and regular communications between the occupational doctor and the individual supervised workers, while the constant feedback between health professionals and hospital psychologists reduced the psychological stress through telematics consulting.
Guarantee of Life-Saving Therapies
The hospital retained the essential hospital services concerning the following medical and surgical activities:
(i)General Surgery Unit; (ii) Specialized Surgery Unit; (iii) Transplant Surgery Unit; (iv) Cardiology, Hemodynamic, Cardiovascular Intensive Care Unit; (v) Geriatrics Unit; (vi) Cystic Fibrosis Unit; (vii) Mother-Child Department; (viii) Radiotherapy Unit; (ix) Haematology Unit; (x) Oncology Unit; (xi) Maxillofacial Surgery Unit; (xii) Oral Surgery Unit; (xiii) Neurosurgery Unit; (xiv) Neurology Unit; (xv) Otorhinolaryngology Unit; (xvi) Psychiatry Unit.
Table 1: Personnel Variation.
|
Permanent Staff |
Contingency Staff |
Crisis Staff |
Total Variation |
||||||
|
Intensive Care Unit |
49 |
doctors |
59 |
doctors |
20% |
64 |
doctors |
10% |
31% |
|
23 |
nurses |
37 |
nurses |
61% |
45 |
nurses |
35% |
96% |
|
|
Infectious Disease Department |
14 |
doctors |
21 |
doctors |
50% |
26 |
doctors |
36% |
86% |
|
10 |
nurses |
18 |
nurses |
80% |
35 |
nurses |
170% |
250% |
|
|
Pediatric Infectious Disease Department |
4 |
doctors |
8 |
doctors |
100% |
10 |
doctors |
50% |
150% |
|
10 |
nurses |
16 |
nurses |
60% |
20 |
nurses |
40% |
100% |
|
|
Mother-Child Department |
37 |
doctors |
40 |
doctors |
8% |
42 |
doctors |
5% |
14% |
|
30 |
nurses |
37 |
nurses |
23% |
44 |
nurses |
23% |
47% |
|
|
Diagnostic Imaging Department |
7 |
doctors |
9 |
doctors |
29% |
11 |
doctors |
29% |
57% |
|
7 |
nurses |
8 |
nurses |
14% |
9 |
nurses |
14% |
29% |
|
|
Internal Transportation System |
10 |
doctors |
12 |
doctors |
20% |
14 |
doctors |
20% |
40% |
|
10 |
nurses |
15 |
nurses |
50% |
16 |
nurses |
10% |
60% |
|
|
Total Personnel |
211 |
280 |
33% |
336 |
27% |
59% |
|||
Table 2: Dressing and Undressing Procedures.
|
Dressing Procedure |
Undressing Procedure |
|
Remove all jewelry and personal items |
Remove the disposable gown and dispose of it |
|
Practice hand hygiene with soap and water or alcoholic solution |
Remove the first pair of gloves and dispose of them |
|
Check device integrity, do not use damaged |
Remove the glasses and sanitise them |
|
Devices |
Remove FFP2/FFP3 by handling it from the rear and dispose of it in the container |
|
Wear a first pair of gloves |
Remove the second pair of gloves |
|
Wear the disposable gown over the uniform |
Practice hand hygiene with alcoholic solutions or with soap and water |
|
Wear FFP2/FFP3 |
|
|
Wear protective glasses |
|
|
Put on a second pair of gloves |
To ensure life-saving assistance and biocontainment of confirmed or suspected cases, was created a filtering system to reduce the risk connected to the hospital access for asymptomatic Covid-19 positive patients. The system was divided in two phases: (i) Pre-Admission Audit and
(ii) Screening on Site [20]. The Pre-Admission Audit was performed by telephone for all patients on the waiting lists, by a healthcare worker who fill out a form investigating the epidemiological and clinical context. The simultaneous presence of epidemiological and clinical criteria, identified a patient at risk. In that event, the patient was denied access to the facility and the required clinical or surgical care procedures were rescheduled, with a process that included a follow-up schedule at 5-day intervals. In the absence of risk criteria, the patient was invited to go to the facility, accessing through an independent and isolated screening area, outside the building, avoiding contamination of the facilities. The screening pathway was one-way and mandatory.
Discussion
In the healthcare system around the world there has been a vital need to develop strategies to survive the Covid-19 pandemic for both infected and non-infected patients requesting life-saving therapies. The preparation of the healthcare system was only possible thanks to the anticipation and planning of surge capacity strategies which have allowed to increase the care capacities of the hospitals, to guarantee the bio-containment and the delivery of healthcare essential to non-Covid-19 positive patients. The planning and governance tool drawn up by the Task Force of the University Hospital “Federico II”, the HIMS, was developed on the basis of the improvement of the hospital response to mass accidents.
However, the non-application of predictive mathematical models is a limitation for the assignment of beds. Indeed at the time, Covid-19 spread rapidly, affecting thousands of patients and hundreds of territories. Therefore, the goal was to expand production capacity as much as possible, avoid paralysis of hospital functions to the detriment of more correct predictive management. Furthermore, during the development of these strategies, it was not possible to make an international, national or local comparison to assess the effectiveness of the interventions implemented, for this reason the HIMS system was evaluated on January 2021 using indicators of productivity for Covid-19 and clinical indicators for life-saving therapies. The hospital productivity indicators during the first year of the pandemic have been calculated on an annual basis (year 2020) as established on national level for the reimbursement frequency for healthcare expenses incurred by hospitals. The clinical indicators to evaluate the provision of life-saving therapies were calculated for the first half of 2020, because during the year the provision of assistance underwent significant and sudden changes in relation to the need to guarantee availability and human resources to patients affected by Covid-19. In Italy, a hospital that admits patients produces healthcare as a final product and must be reimbursed for the expenses it incurs. Diagnosis-related groups (DRGs) are part of an internationally recognized system for hospital reimbursement/funding based on the classification of patients into groups according to the costs consumed during their hospitalization, which depend on their clinical characteristics and the services provided to them [21]. The DRG average relative weight is 1.0. DRGs with a relative weight of less than 1.0 are less resource-intensive and are generally less costly to treat. DRG’s with a relative weight of more than 1.0 generally require more resources and are more expensive to treat. The higher the relative weight, the more resources are required to treat a patient with that DRG. This is why very serious medical situations, such as organ transplants, have the highest DRG weight. Therefore, the indicators used to measure the hospital productivity were the DRG and the DRG weight (Table 3). The data analysis showed that all the hospitalizations, carried out in the areas dedicated to assistance for Covid-19 positive patients, were coded with the Covid DRG (92), furthermore, the average weight was higher than 1.0. This indicates that the complexity of the assistance offered to Covid-19 patients was high and therefore compliant with a third level hospital. The clinical indicators used to measure the ability to guarantee non- deferrable cares despite the pandemic were the following:
(i) number of patients/day for oncological therapies in the Oncology, Haematology and Radiotherapy Unit; ii) number of patients/day for immunological therapies in the Rheumatology and Internal Medicine Units; (iii) number of patients/week for Oncological Surgery; (iv) number of patients/week for Dialysis; (v) number of kidney transplants. The data show a load of activities proportional to those of the same period of 2019 (-20%) without an increase in the waiting lists. These results can be considered suitable with the goal of guaranteeing life-saving therapies (Table 4). We have reported our brief experience which refers to the period from February 2020 to April 2020, in the midst of an emergency. In the absence of a national support health plan, we overall managed to offer 38 beds per medical area (capacity increased by 95%), 8 beds per Intensive Care area (conversion of 100% of existing beds) and 5 beds per Sub-Intensive area (new creation), at the same time guaranteeing safe assistance for Covid-19 negative patients. We have also been identified as Covid-19 hub for pregnant patiens and children, during an epidemiological period in which the literature could offer only a little scientific support. The results of our study inform physicians, hospital administrators, emergency response personnel, and government agencies about a possible scenario for responding to Covid-19 or a similar event. We hope this review will be helpful to anyone facing a similar challenge.
References
- Li H, Liu SM, Yu XH, et al. Coronavirus disease 2019 (COVID-19): current status and future International Journal of Antimicrobial Agents 55 (2020): 105951.
- Istituto Superiore di Sanità. Sorveglianza integrale COVID-19 in Italia (2020).
- Carenzo L, Costantini E, Greco M, et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia 75 (2020): 9289-9234.
- European Centre for Disease Prevention and Severe acute respiratory syndrome (SARS). In: ECDC. Annual epidemiological report for 2015. Stockholm: ECDC (2017).
- Arpino G, de Angelis C, de Placido P, et al. Optimising triage procedures for patients with cancer needing active anticancer treatment in the COVID-19 era. ESMO Open 5 (2020): e000885.
- Phua J, Weng L, Ling L, et Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. The Lancet Respiratory Medicine 8 (2020): 506-517.
- Ludvigsson Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica 109 (2020): 1088-1095.
- Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among Children in Pediatrics 145 (2020).
- Nunziata F, Bruzzese E, Poeta M, et Health-care organization for the management and surveillance of SARS-CoV-2 infection in children during pandemic in Campania region, Italy. Italian Journal of Pediatrics 46(2020): 170.
- Montella E, Caputi EM, del Core M, et Safety Pathway Design for Patients Not Affected by COVID-19 During the SARS-CoV-2 Pandemic in an Italian University Hospital. Risk Management and Healthcare Policy 13 (2020): 2621-2626.
- Xu X, Yu C, Qu J, et Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. European Journal of Nuclear Medicine and Molecular Imaging 47 (2020): 1275-1280.
- Hick JL, Barbera JA, Kelen GD. Refining Surge Capacity: Conventional, Contingency, and Crisis Disaster Medicine and Public Health Preparedness 3 (2009): S59-S67.
- Adams JG, Walls Supporting the Health Care Workforce during the COVID-19 Global Epidemic. JAMA 323 (2020): 1439.
- Taylor BL, Montgomery HE, Rhodes A, et Chapter
- Protection of patients and staff during a pandemic. Intensive Care Medicine 36 (2010): 45-54.
- Ferioli M, Cisternino C, Leo V, et Protecting healthcare workers from SARS-CoV-2 infection: practical indications. European Respiratory Review 29 (2020): 200068.
- Chirico F, Nucera G, Magnavita COVID-19: Protecting Healthcare Workers is a priority. Infection Control & Hospital Epidemiology 41 (2020): 1117-1117.
- lo Vecchio A, Pierri L, Poeta M, et al. Risk of SARS- CoV-2 Transmission in Health Care Personnel Working in a Pediatric COVID-19 Unit. Hospital Pediatrics 11 (2021): e42-e47.
- European Centre for Disease Prevention and Personal protective equipment (PPE) needs in healthcare settings for the care of patients with suspected or confirmed 2019-nCoV. ECDC: Stockholm (2020).
- Palladino R, Mercogliano M, Fiorilla C, et Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study. International Journal of Environmental Research and Public Health 19 (2022): 9670.
- Long QX, Liu BZ, Deng HJ, et Antibody responses to SARS-CoV-2 in patients with COVID-19. Nature Medicine 26 (2020): 845-848.
- Panagiotopoulos P, Maniadakis N, Papatheodoridis G, et al. An Evaluation of Diagnosis-Related Group (DRG) Implementation Focused on Cancer DRGs in Greek Public Hospitals. PharmacoEconomics – Open 4 (2020): 61-69.