Budd-Chiari Syndrome as A Manifestation of Right Atrium Myxoma
Article Information
Komoni F1, Rakovica L1, Sherifi F1, Hyseni F2*, Vokshi V3, Siddik AB4, Rahman M5, Ahsan E6, Mohamed E7, Guy A8, Ikram S9, Musa J10
1Department of Gastroenterology and Hepatology, University Clinic Hospital of Kosova, Republic of Kosovo
2NYU Langone Health, New York, USA
3Department of Anesthesiology, University Clinical Center of Kosovo, Republic of Kosovo
4Department of Pain Medicine, Mayo Clinic, Jacksonville, Florida, USA
5Department of Neurological Surgery, Mayo Clinic, Rochester, Minnesota, USA
6Stem Cell Therapy and Skeletal Regeneration Lab, Mayo Clinic, Rochester, MN, USA
7Department of Cardiovascular Diseases, Rochester, MN, USA
8Clinical Assistant Professor, Department of Physical Medicine and Rehabilitation, New York University School of Medicine, NYU Medical Center, New York, USA
9Department of Neurological Surgery, Mayo Clinic, Rochester, MN, USA
10Department of Surgery Physiology and Biomedical Engineering Mayo Clinic, Rochester, Minnesota, USA
*Corresponding Author: Fjolla Hyseni Vokshi, Department of Urology, NYU Langone Health, New York, USA
Received: 08 August 2021, Accepted: 23 August 2021, Published: 02 September 2021
Citation: Komoni F, Rakovica L, Sherifi F, Hyseni F, Vokshi V, Siddik AB, Rahman M, Ahsan E, Mohamed E, Guy A, Ikram S, Musa J. Budd-Chiari Syndrome as A Manifestation of Right Atrium Myxoma. Archives of Clinical and Medical Case Reports 5 (2021): 622-628.
Share at FacebookAbstract
Budd-Chiari syndrome (BCS) is a rare condition marked by a number of symptoms due to hepatic venous obstruction. A 40-year-old female patient presented with abdominal pain, distension, and dyspnea. An abdominal ultrasonogram showed hepatomegaly, splenomegaly and ascites. A hypodense mass obstructed hepatic flow suggested thrombus formation in the hepatic and portal veins and suprahepatic part of the inferior vena cava on computed tomography. Transthoracic echocardiography was performed to assess thrombus extension to inferior vena cava and underlying pathological processes. It showed a mass lesion in the right atrium near intra atrial septum about 4 × 3 cm in diameter. The lesion manifested as an intracardiac thrombus extending from the inferior vena cava. After the successful surgical removal, the diagnosis of the mass was confirmed as atrial myxoma by histopathological examinations. We conclude that right atrial myxoma is a rare cause of Budd-Chiari syndrome.
Keywords
Budd-Chiari Syndrome; Atrium Myxoma; Thrombus; Echocardiography
Budd-Chiari Syndrome articles; Atrium Myxoma articles; Thrombus articles; Echocardiography articles
Article Details
1. Introduction
Budd-Chiari syndrome is an uncommon disorder resulting from obstruction of the large hepatic veins or inferior vena cava at the suprahepatic level. Alternatively, this syndrome is characterized by occlusion due to hepatic vein thrombosis or mechanical venous obstruction. Budd-Chiari syndrome is characterized by obstruction of hepatic venous flow at the level of right atrium, inferior vena cava, large hepatic veins, or hepatic venules [1]. The etiopathogenesis of Budd-Chiari Syndrome encompasses a wide range of diseases, including myeloproliferative disorders, polycythemia rubella, sickle cell disease, thrombophilia, nocturnal paroxysmal hemoglobinuria, antiphospholipid syndrome, proteinuria, deficiency of protein C and S, antithrombin III deficiency, factor V Leiden mutation) [2, 3].
Any obstruction in the venous vasculature of the liver has been referred to as Budd-Chiari syndrome, from the hepatic venules to the right atrium. This leads to increased hepatic sinusoidal pressure and pressure in the portal vein so that blood flow stagnates. Thus, increased portal pressure causes increased filtration of vascular fluid with the formation of ascites and the development of collaterals through alternating veins leading to esophageal, gastric, and rectal varices. Several factors predispose to the development of Budd-Chiari syndrome, including hypercoagulable, inherited, and acquired conditions, as well as a variety of other causes, can be identified in approximately 75% of patients. Intracardiac tumors have rarely been reported as a predisposing cause for the development of Budd-Chiari syndrome, and surgical removal of these tumors is generally a curative treatment for this syndrome [1, 3-6].
Herein, our authors present a case of a 40-year-old female patient with Budd-Chiari syndrome in whom the right atrium myxoma was manifested with worsening of clinical symptoms despite medical treatment therapy.
2. Case Report
On presentation, the patient was female, aged 40 years old. Her primary complaints included abdominal distention surrounding the epigastrium, tiredness, and malaise for around one month, worsening for the last week. The patient reports that after meals, she has abdominal distention and pain in the epigastrium. The pain was rated as 6 on a visual analog scale (VAS) of 1 to 10 and lasted around 1 hour and accompanied by malaise. After the symptoms become unbearable, she seeks medical attention in a nearby private clinic. After an ultrasound examination, hepatosplenomegaly and ascites were identified. She is referred to the Gastroenterology and Hepatology Department of the University Clinic Center of Kosovo for further evaluation and treatment. She denies previous diseases and hospitalizations. She live with her husband and four children. Do not consume tobacco nor alcohol, or any other psychoactive substances.
On physical examination, patient was oriented to time, space, and surrounding people. Physical constitution revealed a normal-appearing female, well-hydrated skin, and superficial mucosa were slightly icteric and normal body temperature. Regional lymph nodes were not palpated. Her pulse rate was 105/min and blood pressure 120/80 mmHg. The respiratory examination was normal. However, on cardiac auscultation, a mid-diastolic click was heard. The abdomen was slightly distended, and weak bowel sounds were heard. On abdominal palpation the liver was palpated 4 cm below the right subcostal arch in the mid-clavicular line. Spleen was also palpated 1 cm below the left subcostal arch.
Laboratory findings revealed a normal erythrocyte sediment (5 mm/h), low erythrocyte count (3.75 × 106 mm3), low hemoglobin (8.4 g/l), normal hematocrit (45,8), elevated white blood cells (15.2 × 106 mm3), normal platelets (303 × 103 mm3), normal creatinine (108 mmol/L), normal glucose levels (5.8 mmol/L), normal urea (6.2 mmol/L), normal albumin (38 g/L), normal total protein (72 g/L), elevated ALT (126 UI/L), elevated AST (63 U/L), elevated unconjugated bilirubin (45.7 mmol/L) and elevated GGT (157 IU/L). Peripheral blood smear revealed normal erythrocytes, increased number of leukocytes, granulocyte dominance with toxic granules, and a left shift. Platelet counts were in a normal range.
Ascites cytologic examination revealed no malignant cells, no microorganisms were isolated and biochemical analysis revealed a transudative fluid. ECG revealed no pathologic changes. Chest X-ray revealed clear pulmonary fields and normal cardiac silhouette. A repeat ultrasonography confirmed the presence of hepatosplenomegaly and ascites in the abdominal cavity.
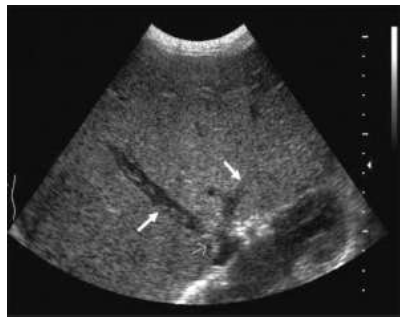
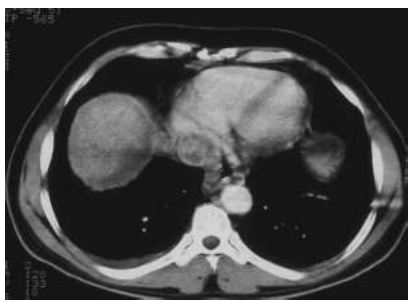
CT with contrast revealed hepatosplenomegaly and additional findings clarifying the pathogenesis of ascites. A hypodense mass obstructed the hepatic flow suggesting a thrombotic process in the hepatic veins, portal vein (PV), and the suprahepatic part of inferior vena cava (IVC).
Gastroscopic examination revealed esophageal varices grade I-II. While undergoing examinations, the patient experiences an episode of thrombophlebitis in the veins of the left lower extremity. In consultation with the vascular surgeon, Fraxiparine 0.3 ml was initiated with clinical improvement within a week. Transthoracic echocardiography was performed to evaluate the extended lesion in the inferior vena cava (IVC) and its relation with cardiac structures. A massive lesion was found in the right atrium, 4 × 3 cm in diameter near the atrial wall. The lesion obstructed the venous flow in the right atrium from the inferior vena cava and limited the diastolic fill of the right ventricle. There was no stenosis nor tricuspid insufficiency. A diagnosis of right atrial myxoma was made.
The patient was released from the clinic with the recommendation to be treated in a more specialized center outside the country. Two months later, the patient returns from the Hospital of Bologna in Italy with a histopathologic diagnosis of right atrial myxoma. Due to the patient's clinical deterioration, she dies 10 months later.
3. Discussion
Budd-Chiari syndrome is a rare clinical disorder characterized by an obstruction of the hepatic venous outlet at any level between the small hepatic venules and the junction of the inferior vena cava, up to the right atrium. This condition results in hepatic congestion, fibrosis, and eventually cirrhosis with portal hypertension. The most common risk factors are hypercoagulable conditions associated with polycythemia vera, myeloproliferative disorders, antiphospholipid syndrome, nocturnal paroxysmal hemoglobinuria, and defects in the coagulation cascade such as deficiency of protein C, S, or C protein.
Most cases of Budd-Chiari syndrome are caused by hepatic vein thrombosis or mechanical obstruction of the venous outlet. The pathological process may be primary when the obstruction of the hepatic venous flow results from a venous endoluminal lesion (thrombosis or congenital disorders) or secondary when the cause of the obstruction is an uncharacteristic external compression by an abscess, cyst, benign or malignant tumor [6-8]. Tumors can cause hepatic venous obstruction by direct invasion or external occlusion. In particular, cardiac tumors are rarely associated with the development of Budd-Chiari syndrome [1, 4]. The clinical presentation of Budd-Chiari syndrome depends on the expansion and rate of venous occlusion, as well as the development of collateral circulation that decompresses the hepatic veins. The syndrome can present as acute, subacute, or chronic. Abdominal pain, hepatomegaly, and ascites are present in almost all patients with BCS. Acute clinical symptoms most commonly include hepatomegaly, pain in the right hypochondrium, nausea, vomiting, jaundice, and ascites [6, 8].
Chronic Budd-Chiari syndrome has been characterized by a history of vague complaints for about six months. Patients may present with complications of cirrhosis and portal hypertension. Laboratory studies generally show findings of chronic liver disease. In our patient, the chronic form was not evident, as it was not presented before the onset of acute symptoms. The patient was in stable condition under medical treatment. However, enlargement of the right atrium myxoma, with narrow localization in the right atrium wall, has caused worsening of the clinical symptoms of chronic BCS. Diagnosis of BCS is based on a combination of clinical and imaging features. The diagnosis of Budd-Chiari syndrome is most commonly diagnosed using noninvasive imaging modalities. Ultrasonographic assessment of the liver and its vasculature is helpful for diagnosis. Doppler ultrasound can detect the localization of obstructions, areas of stenosis, collateral veins, and their proximal dilation may suggest BCS. The diagnostic accuracy of these methods increases if an altered hepatic flow is demonstrated or if the venous flow is absent [9, 10]. Computed tomography is also a widely performed imaging test in the assessment of hepatic veins and liver. A Hypodense filling defects in the lumen of the inferior vena cava and hepatic veins on CT postcontrast images are considered very specific for the diagnosis of thrombosis. Other diagnostic findings include non-visualization of the hepatic vein or inferior vena cava and changes in hepatic parenchyma [4, 11, 12].
50% to 70% of primary cardiac tumors are myxomas [13] commonly in atrium and attached to the interatrial septum of the left atrium. They are slow-growing benign neoplasms that grow from the interatrial septum and expand into the left or right atrium. Approximately 20% of myxomas originate in the right atrium [7, 11, 14]. The right atrium myxoma tends to be more solid with a wider attachment to the atrial wall or atrial septum. In rare cases, atrial myxoma may originate from the inferior vena cava or the junction of the IVC and the right atrium [15-17]. In these rare cases, the risk of developing Budd-Chiari syndrome may be higher. A thrombus in this localization may also mimic a myxoma. Based on literature review, only a few case reports of Budd-Chiari syndrome and portal vein thrombosis are associated with a right atrium myxoma [1, 4, 11]. These cases have been reported with Budd-Chiari syndrome after finding myxoma in the right atrium.
In our case, the tumor exacerbated the clinical symptoms of Budd-Chiari syndrome and the underlying pathological process in the suprahepatic veins. Although atrial myxoma can rarely cause systemic thrombosis, we can conclude that splenic and portal vein thrombosis are associated with predisposing factors. Echocardiography is a beneficial diagnostic imaging modality that can show valvular stenosis or tumor prolapse through the atrioventricular valves. Magnetic resonance imaging and CT imaging are also helpful, allowing mediastinum evaluation and intrathoracic enlargement of the disease process [3, 18]. Magnetic resonance imaging (MRI) is very sensitive in detecting thrombi, which can both visualize the clot and the sequelae. In mediastinal MR imaging, the atrial myxoma is usually a heterogeneous structure with necrotic areas within the tumor. In our case, we did not perform a mediastinal MRI since the patient chose to leave the hospital.
4. Conclusion
Although rare, we have described a case of Budd-Chiari syndrome and portal vein thrombosis caused by a right atrium myxoma, which may be a potential cause of this syndrome. Furthermore, tumors of the right atrium, including myxomas, should be considered in the differential diagnosis of Budd-Chiari syndrome, especially when excluding other causes. Echocardiography can be particularly useful in the diagnostic procedure of patients with Budd-Chiari syndrome.
References
- Anagnostopoulos GK, et al. Budd-Chiari syndrome and portal vein thrombosis due to right atrial myxoma. Ann Thorac Surg 78 (2004): 333-334.
- Khurana A, Tak T. Venous thromboembolic disease presenting as inferior vena cava thrombus extending into the right atrium. Clin Med Res 2 (2004): 125-127.
- Aksu T, et al. Thrombi in the right atrium and inferior vena cava mimicking myxoma in a patient with recurrent pulmonary thromboembolism]. Turk Kardiyol Dern Ars 36 (2008): 555-557.
- Cujec B, et al. Right atrial myxoma presenting as Budd-Chiari syndrome. Ann Thorac Surg 44 (1987): 658-659.
- Scheffel H, et al. Atrial myxomas and thrombi: comparison of imaging features on CT. AJR Am J Roentgenol 192 (2009): 639-645.
- Janssen HL, et al. Budd-Chiari syndrome: a review by an expert panel. J Hepatol 38 (2003): 364-371.
- Onan B, et al. Right atrial myxoma associated with portal and splenic vein thrombosis in a patient with Budd-Chiari syndrome. Turk Kardiyol Dern Ars 39 (2011): 320-324.
- Okuda K. Inferior vena cava thrombosis at its hepatic portion (obliterative hepatocavopathy). Semin Liver Dis 22 (2002): 15-26.
- Even-Sapir E, Iles SE, Barnes DC. Liver scan in Budd-Chiari syndrome. Correlation with CT and Doppler. Clin Nucl Med 18 (1993): 706-708.
- Su L, et al. Clinical Efficacy of Spectral Computed Tomography for Evaluating Liver Function in Patients with Budd-Chiari Syndrome. Acad Radiol 26 (2019): 461-466.
- Grebenc ML, et al. Cardiac myxoma: imaging features in 83 patients. Radiographics 22 (2002): 673-689.
- Sty JR, Starshak RJ, Casper JT. Image correlation. Budd-Chiari Syndrome. Clin Nucl Med, 8 (1983): 369-370.
- Hoffmeier A, et al. Cardiac tumors--diagnosis and surgical treatment. Dtsch Arztebl Int 111 (2014): 205-211.
- Casavecchia G, et al. Cardiac Tumors. J Cardiovasc Echogr 30 (2020): S45-S53.
- Ozer N, et al. Asymptomatic right atrial myxoma originating from the inferior vena cava and right atrium junction in a patient with breast ductal adenocarcinoma. Turk Kardiyol Dern Ars 37 (2009): 479-482.
- Devig PM, Clark TA, Aaron BL. Cardiac myxoma arising from the inferior vena cava. Ches 78 (1980): 784-786.
- Penta de Peppo A, et al. Cardiac myxoma arising from the inferior vena cava. Tex Heart Inst J 19 (1992): 288-290.
- Tsuchiya F, et al. CT findings of atrial myxoma. Radiology151 (1984): 139-143.