Assessment of the Earliness of Detection and Notification of Major Infectious Threats to Global Health Security in Benin
Article Information
Vincent Dossou SODJINOU1,*, Paul Ahoumènou AYELO2, Lamidhi SALAMI3, Alphonse KPOZEHOUEN1, Dona Edgard-Marius OUENDO1
1Regional Institute of Public Health (IRSP), University of Abomey-Calavi, BP 918 Ouidah, Benin
2Medical Sciences Faculty, University of Abomey-Calavi, 01BP 188 Cotonou, Benin
3Ministry of Health, BP 2041 Cotonou, Benin
*Corresponding author: Vincent Dossou SODJINOU, Regional Institute of Public Health (IRSP), University of Abomey-Calavi, BP 918 Ouidah, Benin.
Received: 29 January 2022; Accepted: 07 February 2022; Published: 10 February 2022
Citation: Vincent Dossou SODJINOU, Paul Ahoumènou AYELO, Lamidhi SALAMI, Alphonse KPOZEHOUEN, Dona Edgard-Marius OUENDO. Assessment of the earliness of detection and notification of major infectious threats to global health security in Benin. Archives of Clinical and Biomedical Research 6 (2022): 196-208.
Share at FacebookAbstract
Introduction Early detection and notification can reduce morbidity and mortality from an event. Objective The study assessed the earliness of the detection and the notification of major global health security threats in Benin.
Methods The study was a cross-sectional, descriptive, and analytical. Non-probability sampling and purposive selection of five prone epidemic diseases were used. The earliness of the detection was considered good if at least 80% of cases were detected within 48 hours. This was considered acceptable if at least 80% of cases were detected after 48 hours and before one incubation period of the disease. If none of the two conditions was met, the detection earliness was rated insufficient. The earliness of the notification was judged good if at least 80% of cases were notified within 48 hours. Otherwise, it was deemed insufficient.
Results The early detection of major infectious threats to global health security in Benin was insufficient. No disease threats were detected within 48 hours from 2016 to 2020. Only 72.21% of cases were detected before one incubation period of the selected diseases. Early detection was acceptable for Lassa virus fever and measles. Also, early notification was insufficient. Only 66.22% of cases were notified within 48 hours. The early notification was good for cholera (81.73%), yellow fever (82.13%) and measles (84.14%).
Conclusion Improving rapid access to health services, scaling up electronic reporting and building the capacities of stakeholders on global health security issues are potential means of improvement of detection and notification.
Keywords
Detection; notification; earliness; global health security; Benin
Detection articles, notification articles, earliness articles, global health security articles, Benin articles
Article Details
1. Introduction
Early detection of epidemics enables the reduction of their final scale with lower morbidity and mortality [1] and effective implementation of control measures [2]. In fact, delayed detection of infectious events increases the exposure of new people, generates delays in the response and causes an increase in cases and deaths as reported during the 2014 epidemic of Ebola virus disease (EVD) in West Africa [3]. This delayed detection can compromise the global health security (GHS) in the current context of emerging and re-emerging diseases. Over the detection, early notification is crucial for GHS because it allows the system to take appropriate and timely response measures. Detection and notification fall under epidemiological surveillance domain and their earliness is one of the performance indicators of national surveillance systems.
The earliness of the detection is to be distinguished from the promptness; in fact, promptness is very important in assessing, against a target, the period (of time) between the date of detection of a case and its notification by the person in charge of the surveillance system [4]. The surveillance system has different targets regarding the notification of epidemic prone diseases.
There are diseases that should be immediately notified while other can be notified within one day to one-month periods. When the notification meets these targets, it is prompt or timely. While promptness therefore concerns the ability to meet a specified delay in notification of an event, the earliness of detection relates to the time taken by the epidemiological surveillance system to identify the event. Benin has a surveillance system modeled on the pyramidal structure of its health system.
This surveillance is based on the integrated disease surveillance and response (IDSR) [5]. The first functions of IDSR are detection and notification. Benin is implementing mainly syndromic surveillance, but some diseases require confirmation by the laboratory network. The health system stakeholders are trained and equipped to carry out the surveillance main functions, including detection and notification.
The surveillance system covers all infectious threats to GHS reported in the country. These threats include recurrent epidemics of cholera, meningitis, Lassa virus fever and meningitis on one hand, but also major risks such as yellow fever, EVD, emerging and re-emerging diseases including the current Covid-19 pandemic. Early detection and notification of these events is necessary in the context of GHS. During recent annual self-assessments of the International Health Regulations (IHR) 2005 as well as the joint external evaluation of the IHR 2005 [6], surveillance was identified as one of the strengths among the IHR core capacities in Benin.
This finding is encouraging and indicates that the surveillance system has been able to detect major epidemics. However, to our knowledge, there is no specific evaluation of the early detection and notification of infectious events Benin. To fill this gap and as part of initiatives to strengthen GHS in Benin, this study aims to assess the earliness of detection and notification of major infectious public health emergencies in Benin.
2. Methods and Settings
2.1 Study settings
The study was organized in Benin Republic. The country has 34 health districts in the 12 departments. Surveillance is coordinated at the national level by the National Direction of Public Health (DNSP). At the departmental level, surveillance is implemented by all public health structures under the coordination of departmental public health services. The country has a rich network of private health structures involved in surveillance at different stages. The IDSR national guide describes the surveillance functions in the country; and for each disease, the case definition and the actions expected from surveillance teams.
2.2 Methods
Study design
The study is cross-sectional, descriptive and analytical.
Study population
The study population was the national surveillance system. The target populations were epidemic prone diseases notified between 2016 and 2020.
Sampling
The sampling method was non-probability; a purposive choice was used to select the diseases. This choice was based on criteria namely (i) disease whose final confirmation is ensured by the laboratories, (ii) disease targeted by strengthening project or program for their control, elimination or eradication and (iii) viral hemorrhagic diseases reported in the country during the last five years. Cholera, Lassa virus Fever disease (LVF), measles, meningitis and Yellow fever were then selected. For each disease, all cases notified between 1 January 2016 and 31 December 2020 were included in the investigation.
Data collection
For data collection, an Excel database was developed. The variables in this database included the serial number, the epidemiological number, the notified disease, the notifying township, notifying health district, notifying department, the date of consultation in the health facility (HF), the date of notification by the HF, the date of onset of the disease, the date the samples were collected, the date the samples were sent to the laboratory, the date the samples were received at the laboratory, the date the results were released by the laboratory, the date of receipt of the laboratory results by the notifying HF and the year of notification of the case. Data on the targeted diseases were made available by DNSP. Document exploitation and observation (measuring of delay) were the data collection techniques. The detection and notification delays were calculated by inserting the appropriate formula in the Excel file.
Variables and operational aspects
The dependent variables were the detection and notification of diseases, characterized by their duration. The detection delay was determined by the difference between the date of release of the laboratory results and the date before the onset date of the disease.
This principle enables to consider each night as a whole day. For measles and meningitis, diseases for which the patient is infectious before becoming symptomatic, a corrected detection delay was determined by the difference between the date of release of the laboratory results and the day before the date of onset of the infectious period of the disease. For measles, the patient becomes infectious 4 days before the onset of the rashes, while for meningitis, the patient is infectious 7 days before the onset of the disease. Onset of infectiousness was determined by subtracting 4 days from each case onset date for measles and subtracting 7 days from each case onset date for meningitis.
The notification period was determined by the difference between the date of notification of the case to the first possible structure by the health facility and the day before the consultation date in the health center. Early detection was rated good if at least 80% of infectious threats were detected within 48 hours from the onset date. The detection was deemed acceptable if at least 80% of cases were detected after 48 hours but before one incubation period of the disease. By example, for measles, detection will be considered acceptable if at least 80% of cases are detected after 48 hours and before 14 days after the onset of the disease. Detection was deemed insufficient if any of the two above conditions is met. The notification of the infectious event was considered early if at least 80% of the cases were notified by the health facility within 48 hours after the consultation, regardless of the notified structure [7-8]. Otherwise, the notification was declared late.
Ethical aspects
The study was carried out after the approval of the ethics committee of biomedical sciences of the University of Parakou. Data collection authorization has been submitted to the Ministry of Health and has been approved. The databases made available were anonymized by removing the first and last names of cases and using epidemiological numbers for their identification.
Bias
Data was cleaned with the removal of cases with inconsistent data. Entries for all detection and notification times that gave negative results have been removed from the database.
Data analysis
Stata-14 software was used to perform the statistical analyzes. The times for detection and notification of each case were calculated. The proportion of cases detected before 48 hours was determined and compared to the defined standards. The proportion of case detected after 48 hours was also calculated and compared to one incubation period. Results were reported as the median followed by the interquartile range (Q1, Q3) for quantitative variables as the distribution was not normal. The Kruskal Wallis test was used to compare the differences between the groups. Significance levels were set at 5% (p <0.05).
3. Results
A total of 5,511 records of cases of targeted diseases were available. The database included 106 cholera records, 805 suspected Yellow fever records, 39 Lassa viruses Fever; 1,993 meningitis records and 2,568 suspected measles cases. After data cleaning, a total of 5,124 records were maintained; these included 104 for cholera, 800 for Yellow fever, 39 for Lassa virus Fever; 1,930 for meningitis and 2,251 for measles.
3.1 Detection delay of infectious emergencies
The overall detection median delay for the five targeted diseases was 8 (6; 11) days. The extremes include a minimum of 3 days and a maximum of 65 days. Tables I shows the detection median delays by department.
This median delay varies from 4 (4; 5) for cholera to 9 days for yellow fever and measles (Table I). The analysis by department shows that the detection median delays vary from 7 days in the four northern departments to 10 days in Couffo department. Four departments have a median delay higher than the national median (Table I).
There was significant difference nationally between the disease detection delays (p = 0.000). Yellow fever and measles were the diseases with the longest detection periods. There was also a significant difference between regions for detection delay (p = 0.000).
Couffo, Mono, Ouémé and Plateau were the departments with the longest detection periods. By disease, there was no significant difference between the departments for the detection of cholera (p = 0.245) and Lassa virus fever (p = 0.458). But there was a significant difference for yellow fever (p = 0.004), meningitis (p = 0.000) and measles (p = 0.000)
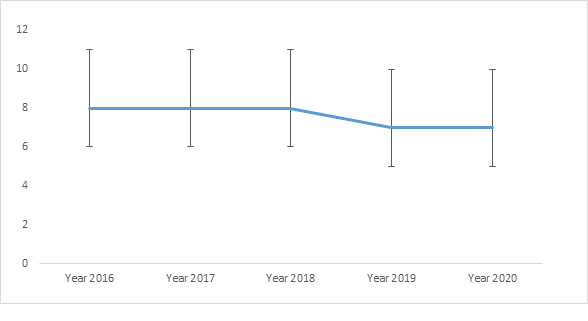
Table II presents the detection delay and the notification delay trend per year for each disease and globally. The overall detection delay shows a downward trend between 2018 and 2019 with a stabilization between 2019 and 2020 (figure 1).
Table I: Median time to detection and median time to notification of major infectious public health emergencies by department, disease, for all diseases and for the whole country, Benin, November 2021.
*DD: Detection delay **ND: Notification delay ***-: No reported case
Table II: Evolution by year of the detection median delay globally and by disease, Benin, 2016 to 2020.
*DD: detection delay **ND: notification delay ***-: No reported cases
3.2 Corrected detection delay
The overall median time of detection, corrected was 13 (12; 16) days for meningitis and 12 (11; 15) days for measles. The overall median time of detection corrected for these two diseases was 13 (11; 15).
3.3 Assessment of early detection
There was no case of targeted epidemic-prone diseases detected within 48 hours. The early detection was therefore not good; A proportion of 71.08% of the cases (3,642) of these targeted diseases were detected after 48 hours and before one incubation period of each of the targeted diseases (Table III). The early detection of infectious threats to global health security in Benin was therefore insufficient. The early detection was however acceptable for cholera (90.40%), Lassa virus fever (89.74%) and measles (84.85%).
3.4 Assessment of the earliness of syndromic detection
A total of 2,316 cases (45.19%) were suspected within 48 hours; 4,666 cases (91.06%) were suspected after 48 hours and before one incubation period. The early syndromic detection was acceptable. The earliness of syndromic detection was good for cholera (95.19%); and acceptable for LFV (94.87%), meningitis (95.91%) and measles (94.71%). It was insufficient for yellow fever.
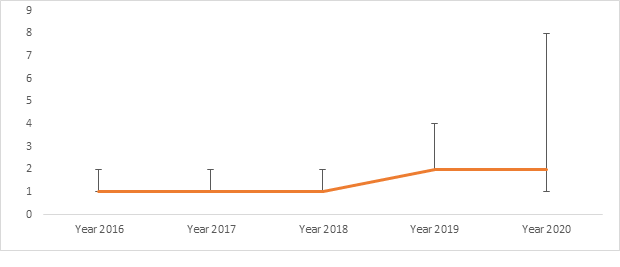
3.5 Notification of infectious emergencies
The overall notification median time for the five targeted diseases was 2 (1; 3) days (Table I). The minimum delay was 1 day, and the maximum was 74 days. The median notification duration per year doubled between 2018 and 2019 and stabilization was seen between 2019 and 2020. On other hands, the third quartile tripled between 2019 and 2020 (Figure 2).
3.6 Assessment of the earliness of the notification
A total of 3,391 cases (66.17%) were notified within 48 hours (Table III). The notification of infectious threats to health security was therefore late. There was significant difference at the national level between the notification delays (p = 0.000). Meningitis was the disease with the longest notification delay. There was also significant difference between departments for notification period (p = 0.000). Borgou and Ouémé were departments with the highest notification periods for all targeted threats. Specifically, there was significant difference between regions for notification of yellow fever (p = 0.000), meningitis (p = 0.000) and measles (p = 0.000). For the other diseases, there was no difference.
Table III: Results of the evaluation of the earliness of detection and notification of GHS infectious threats from 2016 to 2020 in Benin.
4. Discussion
The objectives assigned to this study were achieved. The earliness of the detection and the notification of major infectious threats to GHS in Benin was assessed. The diseases selected were representative of major infectious emergencies in Benin and the assessment over five-year period allows an objective assessment of the situation.
4.1 Detection delay of major infectious emergencies
Half of the cases of targeted diseases were detected after 7 days. This situation reflects a potential late detection of epidemics with high risks of spread of infectious threats. However, the median delay found in our study is lower than the median delay of 27 days found by Kluberg et al. in Africa between 1996 and 2014 [9]. It is also lower than the estimated median delay of 12 days found in Canada [10], as well as the 13.5 days reported by Chan in 1996 worldwide [11] and the 8 days registered by Mersini in Europe [12]. This performance can be explained by the capacity building of stakeholders on the implementation of IDSR; and by the fact that the surveillance of targeted diseases is reinforced by specific programs and projects. Median delays vary from 3 days for cholera to 8 days for yellow fever and measles. These detection times are less than the 10 days found by Yoo et al for yellow fever and dengue in Korea [13]. The median delays for detection of Lassa virus fever, yellow fever and measles are greater than the 5 days found by Yoo for shigellosis; however, the detection delay of cholera was better than shigellosis detection delay in Yoo's study [13]. While these are two diarrheal diseases, the occurrence of recurrent epidemics in Benin has led to the strengthening of cholera surveillance with better detection delay. Overall, detection delays for 71% of cases are less than one incubation period. This means that 7 out of 10 patients are detected before their first contacts become infectious. This finding is very encouraging because the calculated deadlines included biological confirmation delay in a country where public health actions begin as soon as events are suspected. The detection delays in our study are impacted by the consultation delays.
The overall median consultation delay for the targeted diseases was 3 (1; 5) days. The unsuitable therapeutic itinerary with the self-medication or seeking care from traditional healers at first stage of the disease explains these delays in consultation [14]. The country's health system must strengthen risk communication measures, health insurance mechanisms and the geographical accessibility of communities to health services to reduce consultation delays and facilitate early detection of public health emergencies. In addition to the consultation delays, the long detection delays can be explained by the insufficient knowledge of surveillance stakeholders on case definitions, especially in the private sector and at community level. Out of 94 structures assessed, case definitions were found in 65 structures (69%) including just 5 private structures; these case definitions were present in the disease consultation room in only 45 health centers. Finally, the lack of a functional event-based surveillance can also explain the high detection times. In fact, according to other authors, informal sources enable the detection of information 1.26 days earlier than formal sources [15].
Early detection
The overall earliness of detection was insufficient for all targeted threats. There was no case detected within 48 hours after disease onset. Other authors reported similar situations with low proportion of epidemics detected within 48 hours. Thus, Dato et al, in a review covering the period from 1993 to 2000, found that only five epidemics out of 51 had been detected within 48 hours in the United States [16]. On other hands, about 30% of cases were not detected until their first contacts become ill in our study. This situation is more worrying for meningitis and measles, for which the family and social contacts are exposed for 13 days to patients in active transmission period. In these situations, it will be difficult to prevent the occurrence of several generations of cases, especially in a context where contact tracing is not systematic for some diseases. The low proportion of cases detected before one incubation period could be explained by confounding factors or specificities related to some diseases. By example, for Yellow fever, the onset of jaundice can occur between the second and the fourteenth day after the fever. Also, malaria endemicity in the country with severe icteric malaria forms may also explain the delay in suspecting yellow fever; insufficient knowledge on case definitions is another reason for insufficient status of the detection earliness. The trend in median detection delays shows a decrease between 2018 and 2019 followed by stabilization. The observed decline is consistent with Chan's findings at the global level. According to his observations, the time taken to detect epidemics has been reduced from 28 days before the implementation of the IHR to 7 days after its implementation [11]. The stabilization observed between 2019 and 2020 may be linked to the Covid-19 pandemic which caused a disruption in the supply of essential services; a mobilization and absorption of resources from the health system, leading to a decline in the performance of other programs including surveillance [17]. Strengthening the continuity of services to other threats to GHS will enable improvements in mechanisms for early detection of events and maintain the decrease in detection delays seen since 2018. Statistical analyzes have shown significant differences between diseases and departments. Cholera is detected faster than other targeted diseases. This could be explained by the acute nature of the disease but also by a greater community awareness of the impact of the disease. Patients affected by cholera seek care faster than others. The departments of Ouémé, Plateau, Mono and Couffo had the longest detection times compared to the others. This finding seems absurd. Indeed, these departments are among those with the best availability in health structures and human resources compared to the departments of the northern part. In addition, they are very close to Littoral department (where the national reference laboratory is located) and have better facilities for the transport of samples. An in-depth study including an anthropological component would be necessary to identify and analyze the reasons of low performance reported from these departments. In general, building the capacity of structures and stakeholders on GHS issues and on the importance of early detection is urgent. The weaknesses found seem to be more human than structural. The country has a well-established and functioning surveillance system with clear technical guidelines. Public health measures are initiated as soon as the cases are suspected. But the commitment of stakeholders that are running the system must be more tangible for the effectiveness of the earliness of the detection in the country. The surveillance of the diseases targeted in this study are supported and enhanced by specific surveillance programs or projects. Despite this, the early detection is insufficient. This situation is potentially indicative of longer detection times for other threats, including new events. The integration of surveillance, especially the samples transportation to laboratories, is not always effective; in fact, some diseases are not always taking advantage of surveillance mechanisms established for the diseases targeted in this study.
Earliness of the notification
The proportion of targeted threats notified within 48 hours in our study was better compared to other studies. By example, the proportion of measles cases notified within 48 hours was higher than the proportion of 28% found in Qatar in 2008 [18]. The median delay of 4 days for meningitis was better than the 12 days reported for meningitis by Jajosky in the United States [19]. The median duration of 1 to 4 days found was better than the duration of 6 to 20 days found by Yoo et al in Korea [13] for the notification of 6 diseases; than the 26 to 36 days found for the surveillance of enteric diseases by Galanis et al in Canada [10] as well as than the 4 days found in Europe by Mersini [13]. In addition to the median delays, the proportion of cases notified before one incubation period (75%) was also better than the 40% found by Jajosky [19]. Despite these findings, the overall earliness of the notification in our study was insufficient. This insufficient delay is negatively impacted by the low proportions of Lassa virus fever and meningitis cases notified within 48 hours. The overall insufficient notification earliness found in our study is similar to the findings of several studies. Swaan et al. found also that only 11 of 48 studies showed good notification times [7]. The weaknesses of electronic notification in Benin can explain the late notification. Electronic notification has been shown to reduce notification and action times [7, 20]. However, the notification is still to a large extent based on papers in Benin.
Notification times doubled between 2018 and 2019. Such an increase in the context of major epidemics of emerging and re-emerging diseases at the regional and global level, is concerning. Notification is essential to trigger response measures by public health structures. The increase in the notification period will generate a delay in decision-making and initiation of response measures. A thorough analysis of the underlying factors of this increase is needed. Obviously, dysfunctions were persisting before the onset of Covid-19 and were aggravated as observed for other health services [17]. As mentioned above, the reported trends are more linked to human behaviours and commitment than structural or organizational problem. The country has syndromic surveillance with clear targets for notification of suspected cases. The events notifications are most often made even before the biological confirmation. In this context it is difficult to understand the late delays found in notification. This is more worrisome as the notification delays in this study were calculated from the date of notification by the health facilities and not from the date of reception of the notification by the notified structure. Capacity building of surveillance stakeholders on the importance of early notification is needed. Also, the establishment of an electronic notification platform must be accelerated for the real-time reception of notifications by decision-making structures.
5. Conclusion
The early detection of infectious threats to health security in Benin was insufficient. There was no case detected within 48 hours and less than 80% of cases were detected before one incubation period. Detection times were acceptable for cholera, Lassa virus fever and measles. The notification was early for cholera, yellow fever and measles. But the overall notification of GHS threats was late. Strengthening the continuity of services in the current context of Covid-19, strengthening the capacities of private sectors and community-based surveillance stakeholders, the remobilization and motivation of human resources; and the strengthening of electronic notification at the national level are potential means of improving the early detection and notification of infectious threats to GHS in Benin.
References
- Steele L, Orefuwa E, Dickmann P. Drivers of earlier infectious disease outbreak detection: a systematic literature review. Int J Infect Dis 53 (2016): 15–20.
- Farrington CP, Andrews NJ, Beale AD, Catchpole MA. A Statistical Algorithm for the Early Detection of Outbreaks of Infectious Disease. J R Stat Soc Ser A Stat Soc 159 (1996): 547–63.
- World Health Organization. Ebola situational report of 10 June 2016 (2016): 2p.
- Mata E. Surveillance System of Infection Diseases and Vaccination in Albania: Evaluation (2011): 219p.
- World Health Organization. Technical guidelines for the integrated disease surveillance and response (IDSR) 2010 (2010).
- World Health Organization. Joint external evaluation of IHR core capacities of the Republic of Benin: mission report (2017): 50p.
- Swaan C, Broek A, Kretzschmar M, Richardus JH. Timeliness of notification systems for infectious diseases: A systematic literature review. PLOS ONE 13 (2018): e0198845.
- World Health Organization. Joint External Evaluation tool - second edition. 2018. Geneva. World Health Organization. 122p.
- Kluberg SA, Mekaru SR, McIver DJ, Madoff LC, Crawley AW, Smolinski MS et al. Global Capacity for Emerging Infectious Disease Detection, 1996-2014. Emerg Infect Dis 22 (2016): E1 – 6.
- Galanis E, Taylor M, Romanowski K, Bitzikos O, Jeyes J, Nowakowski C et al. Evaluating the Timeliness of Enteric Disease Surveillance in British Columbia, Canada, 2012-13. Can J Infect Dis Med Microbiol. 2017 (2017): e9854103.
- Chan EH, Brewer TF, Madoff LC, Pollack MP, Sonricker AL, Keller M et al. Global capacity for emerging infectious disease detection. Proc Natl Acad Sci 107 (2010): 21701–6.
- Mersini K, Sulo J, Agolli L, Vasili A, Musa S, Kunchev A et al. Evaluation of main infectious diseases outbreak detection and response timeliness in Southeast European Region. Int J Infect Dis 79 (2019): 129.
- Yoo HS, Park O, Park HK, Lee EG, Jeong EK, Lee JK et al. Timeliness of national notifiable diseases surveillance system in Korea: a cross-sectional study. BMC Public Health 9 (2009): 93.
- Mariam MD, Djeneba ON, Mireille D, Koumavi E. La mesure de l’usage de la médecine traditionnelle en Afrique de l’Ouest. Revue Bio-Africa 18 (2018): 42 – 56.
- Bahk CY, Scales DA, Mekaru SR, Brownstein JS, Freifeld CC. Comparing timeliness, content, and disease severity of formal and informal source outbreak reporting (2015).
- Dato V, Wagner MM, Fapohunda A. How outbreaks of infectious disease are detected: a review of surveillance systems and outbreaks. Public Health Rep 119 (2004): 464–71.
- Masresha BG, Luce R, Shibeshi ME, Ntsama B, N’Diaye A, Chakauya J et al. The performance of routine immunization in selected African countries during the first six months of the COVID-19 pandemic. Pan Afr Med J 37 (2020): 12.
- Nazzal ZA, Said H, Horeesh NA. Measles surveillance in Qatar, 2008: quality of surveillance data and timeliness of notification. East Mediterr Health J 17 (2011): 813 – 7.
- Jajosky R, Groseclose S. Evaluation of Reporting Timeliness of Public Health Surveillance Systems for Infectious Diseases. BMC Public Health 4 (2004): 29.
- Quan V, Hulth A, Kok G, Blumberg L. Timelier notification and action with mobile phones–towards malaria elimination in South Africa. Malar J 13 (2014): 151.