Assessment of the Countries’ Readiness to Detect and Control Cholera Outbreaks in the WHO African Region
Article Information
Vincent Dossou Sodjinou1*, Mory Keita1,5, Dick Chamla2, Jean Paul Kimenyi2, Fiona Braka2, Ambrose Talisuna2, Harsh Lata3, Guy Mbayo2, Fred Kapaya4, Tamayi Mlanda2, Nannie Ishata Conteh2, Abdou Salam Gueye2
1World Health Organization, Regional Office for Africa, Dakar Emergency Preparedness and Response Hub, Senegal
2World Health Organization, Regional Office for Africa, Brazzaville, Congo
3World Health Organization, Headquarter, Geneva, Switzerland
4World Health Organization, Regional Office for Africa, Nairobi Emergency Preparedness and Response Hub, Kenya
5University of Geneva, Institute of Global Health, Geneva, Switzerland
*Corresponding author: Vincent Dossou Sodjinou, World Health Organization – Dakar Emergency Preparedness and Response Hub, BP 4039 Dakar, Senegal.
Received: 22 July 2022; Accepted: 01 August 2022; Published: 17 August 2022
Citation: Vincent Dossou Sodjinou, Mory Keita, Dick Chamla, Jean Paul Kimenyi, Fiona Braka, Ambrose Talisuna, Harsh Lata, Guy Mbayo, Fred Kapaya, Tamayi Mlanda, Nannie Ishata Conteh, Abdou Salam Gueye. Assessment of the Countries’ Readiness to Detect and Control Cholera Outbreaks in the WHO African Region. Archives of Clinical and Biomedical Research 6 (2022): 656-662.
Share at FacebookAbstract
Objective: This study assessed the countries’ readiness to prevent, detect, respond and recover from cholera outbreaks.
Methods: This descriptive and cross-sectional study targeted 28 countries at risk of cholera. A readiness tool, covering all pillars required by the global health security was developed. Criteria, fit-tested with the regional framework for cholera elimination by 2030, were defined for each pillar. Based on experts’ opinion, each pillar and corresponding criteria were weighted. Data was collected in each country through group discussion of multi-sectoral cholera teams. The data collected were analyzed and visualized through an online Power BI tool. The readiness for each pillar was rated good if the pillar assessment result reached at least 80 % of expected points. The readiness was moderate if ranging between 50 % and 80 %. The readiness was limited if the rating was below 50%. The readiness status of each country was based on the same criteria.
Results: The overall countries’ readiness level to detect and respond to cholera was insufficient. Of the 23 responding countries, there was no country with good readiness. Seven countries had moderate readiness while sixteen had limited readiness level. Laboratory was the best performing pillar with good readiness reported in eight countries. Only three countries had good readiness level for surveillance, two countries for infection prevention and control, and one country respectively for coordination and, water sanitation and hygiene.
Conclusion: Countries in the WHO African Region were not adequately prepared to prevent or control cholera outbreak. Such readiness assessment provided critical information about areas of improvement across the 11 pillars and should be regularly undert
Keywords
Cholera; preparedness; readiness; WHO African Region
Article Details
1. Introduction
Cholera remains one of the most frequent public health emergencies reported in the World Health Organization (WHO) African Region [1]. Even though the burden of cholera in underreported, it still remains the highest in the region, with at least 10 Member States (MS) reporting cholera outbreaks every year. In 2021, a total of 137,116 cases and 4,062 deaths (case-fatality ratio (CFR) of 3.0%) were reported in 19 countries in the Region. This figure was mainly driven by the largest cholera outbreaks reported in West Africa and that culminated in a total of 108,859 cases and 3,711 deaths (case fatality ratio of 3.4%) reported from 4 January 2021 to 14 November 2021 in seven countries [2]. Cholera is a well-known disease for which evidenced-based interventions are known. In 2017, stating that cholera deaths can be prevented by tools that are available today, the Global Task Force on Cholera Control (GTFCC) adopted the strategy “Ending cholera: A global roadmap to 2030” [3]. One year later, WHO African MS endorsed the framework for the implementation of the global strategy for cholera prevention and control 2018 – 2030 [4]. The frameworks define targets and milestones for countries. The achievements of these milestones and of the overall goal of eliminating cholera need proper preparedness of countries and their readiness to prevent, detect and respond to cholera outbreaks. Since the outbreak of Ebola virus disease (EVD) in West Africa in 2014–2016 and the response to other outbreaks and complex emergencies, WHO has undertaken major reforms to its emergency programme to prepare it to address global health security challenges [5]. In line with these reforms, WHO developed rigorous methods and procedures ensuring that guidelines and assessments tools are evidence-based and meets the highest internationally recognized standards to be credible, trustworthy and relevant to end-users [6]. One such example was the development of the EVD consolidated checklist during the Ebola outbreak [7]. This checklist was used by WHO and partners to organize the preparedness strengthening teams’ (PST) missions in different countries [8-10]. These PST missions were instrumental in increasing the readiness of Guinea, Liberia and Sierra Leone neighboring countries as well as other countries at risk of EVD in being ready to prevent, detect and respond to EVD. Outcomes of these missions included timely detection and quick controls of EVD outbreaks in Mali and Senegal. Building on these positive outcomes, the decision to develop a readiness checklist for cholera was made. In fact, according to WHO, high-level operational readiness to respond to emergencies will allow a timely, effective, and efficient response. Achieving readiness is a continuous process of establishing, strengthening, and maintaining a multisectoral response infrastructure that can be applied at all levels, which follows an all-hazard approach, and which focuses on the highest priority risks. Operational readiness builds on existing capacities to design and set up specialized arrangements and services for an emergency response [11]. This is crucial for global health security (GHS) and international health regulations (IHR). Cholera is one of the three infectious diseases targeted by IHR in 1969 [12]. The disease is therefore of highest interest for the GHS. The recent burden of cholera outbreaks in the African Region and in humanitarian settings such as Haiti, Yemen, Pakistan have raised again the need for better preparedness and readiness of countries to better prevent, detect and respond to the outbreak and mitigate its socioeconomical impact. During the 2021 cholera outbreaks in West Africa and the cross border spread that was being documented, the countries at highest risk of cholera were identified across the Region. This assessment was conducted in these countries to monitor their readiness level and identify major areas of improvements. For this purpose, a readiness assessment tool was developed to identify gaps to be filled for a better response to present and future epidemics. This paper summarizes the findings of this assessment.
2. Settings
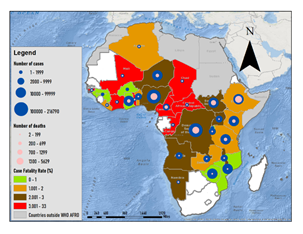
The Study was conducted in the WHO African Region that covers 47 Member States. Cholera is endemic in some countries across the Region with outbreaks frequently reported. From 2014 to 2020, a total of 742,977 cases of cholera and 15,020 deaths (CFR: 2.0%) were officially reported in the Region according to the WHO cholera annual reports available in the WHO weekly epidemiological records. The region accounted for 21% of all cases reported globally during this period but more importantly for more than 80% of all deaths globally. A total of 29 Member States were affected by cholera outbreak, at least one time, during this period (Map 1).
3. Methods
3.1 Study Design
This study is descriptive in design and cross-sectional in nature. It included the WHO AFRO countries that were at risk of cholera during the 2021-2022 outbreak. The main criteria were (i) cholera prone countries, (ii) countries at risk of spread from countries affected by cholera outbreaks and (iii) countries affected by flood or humanitarian situation. A total of 28 Member States were identified and included in the study.
3.2 Data Sources and Measurement
The collection tool was an excel sheet developed by the WHO African Region Emergency Preparedness and Response (EPR) cluster through an iterative process. A multidisciplinary and multisectoral team was established to develop and validate the assessment tool. The tool covers all pillars required to control an emergency in the context of GHS. These pillars included (i) coordination, (ii) rapid response team (RRT), (iii) surveillance, (iv) laboratory, (v) point of entry (PoE), (vi) case management, (vii) infection prevention and control (IPC) and safe burials, (viii) risk communication and community engagement (RCCE), (ix) logistic and procurement, (x) vaccination, (xi) water, sanitation and hygiene (WASH) and food safety. The tool was developed in English and in French. The tool contains two sheets. One in intended to collect baselines information on the pillars such as number of districts in the country, number of hotspots etc. The second sheet is for the assessment. The dataset includes (i) criteria, (ii) status (yes or no), (iii) deadline to implement corrective actions if criteria were not met, (iv) comments and (v) people responsible for the implementation of corrective actions if criteria were not met. The questions in the tool were also tailored to the requirements of the Regional framework for the implementation of the global strategy for cholera prevention and control 2018 – 2030 endorsed by WHO Member States in August 2018 in Dakar, Senegal. A list of criteria was defined for each pillar for the assessment leading to a total of 69 criteria assessed. The study was a self-assessment performed by each country. Focus Group discussion was the data collection technique. A multidisciplinary team comprising of Ministry of Health cholera multidisciplinary stakeholders, Ministries of water focal persons for WaSH, WHO; and local and international partners convened meeting to discuss and assign binary (yes/no) responses to the questionnaire. The filled sheet was shared with the WHO African Region cholera team for analysis. Data collection was conducted from 6 December 2021 to 14 March 2022.
3.3 Data Management and Analysis
The data collected was analyzed by an analysis Excel platform developed to generate the assessment result. A Power BI based tool enabled visualization of the results. The results were generated for each pillar as well as a global result for all pillars for each country. Data analysis started by an experts’ opinion to weight each pillar. The subject matter experts’ team was comprised of staffs and consultants from the Regional Office for Africa and of the main cholera prone countries. Based on the prior knowledge and consultative process, each pillar was assigned a weight to reflect their relative importance in assessing readiness for cholera by the subject matter experts’ team (table 1). Inside each pillar, each question/criterion was also weighted. An expected total number of points for each pillar was determined based on the questions’ weight and the assumption that all criteria would be met. During the analysis process, each pillar question with positive response was granted one point or zero for negative response. An overall pillar readiness result was then calculated as the sum of the weighted result of each pillar question. The readiness level for each pillar was rated “good” if the pillar assessment result (total points) reached at least 80 % of expected points. The level was rated “moderate” if the pillar assessment result ranged from 50 % to 80 %. The level was “limited” if the pillar assessment result was less than 50%. Similarly, the overall country readiness assessment result was calculated as the sum of the weighted results of each pillar. The overall readiness level of a given country was rated “good”, “moderate” or “limited” if the overall country readiness assessment result (total points) reached at least 80 %, 50% to 80% or less than 50% of the total expected points of the assessment, respectively.
|
Pillar |
Number of criteria |
Weight of the pillar |
|
Coordination |
10 |
15.20% |
|
Rapid Response team |
4 |
10.10% |
|
Surveillance |
7 |
12.60% |
|
Laboratory |
8 |
9.40% |
|
Point of entry |
6 |
5.80% |
|
Case management |
4 |
9.30% |
|
Infection prevention and control; safe burials |
7 |
8.90% |
|
Risk communication and community engagement |
6 |
7.90% |
|
Logistic and procurement |
5 |
5.20% |
|
Vaccination |
4 |
3.80% |
|
WASH and food safety |
8 |
11.70% |
Table 1: Number of criteria assessed pillars and weight of each pillar during analysis, WHO African Region, March 2022.
4. Results
The checklist was shared with 28 countries, of which 23 countries completed the assessment. These included nine countries from West Africa (Benin, Burkina Faso, Cote d’Ivoire, Ghana, Mali, Niger, Senegal and Sierra Leone), three from Central Africa (Cameroon, Chad and the Democratic Republic of Congo (DRC)) and eleven countries from Eastern and southern Africa (Ethiopia, Kenya, Malawi, Madagascar, Mozambique, Namibia, South Sudan, Uganda, United Republic of Tanzania, Zambia and Zimbabwe).
4.1 Readiness Level by Different Pillars
The results by pillars as well as the overall score for each country are showing in table 2. Apart from the laboratory pillar, more than half of the countries had limited readiness level per pillar. For laboratory pillar, eight countries had good readiness level and seven had moderate level. In surveillance pillar, three countries had good readiness level and six had moderate level. For the infection prevention and control pillar, two countries had good readiness level while nine had moderate readiness level. One country had good readiness level in coordination while eight other had moderate readiness. One country had good readiness level and five had moderate level for WASH pillar. In six countries (Burkina Faso, Ghana, Malawi, Mali, Mozambique, Uganda), there was just one pillar that reached good readiness level. Three countries (DRC, Ethiopia, Rwanda) had two pillars with good readiness capacity while Tanzania reported three pillars with good capacities. In thirteen countries, there was no pillar that had good readiness level (table 2).
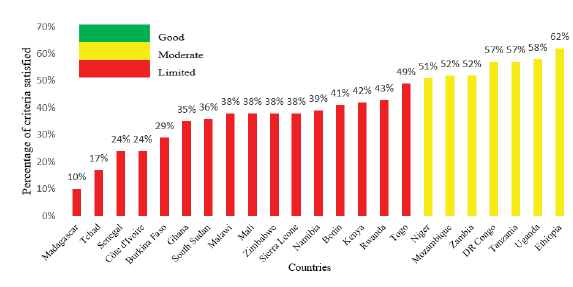
4.2 Readiness Level in Different Countries
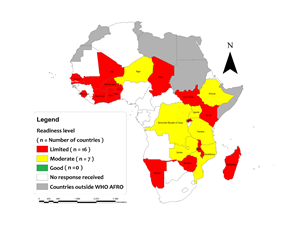
The overall readiness score per country ranged from 10% in Madagascar to 62% in Ethiopia (table 2, figure 1). There was no country that had good overall readiness capacity. Only seven (30.3%) countries had moderate capacity in the region while sixteen (69.7%) countries had limited overall readiness level (table 2, map 2).
Table 2: Countries Cholera Readiness Assessment Results, WHO African Region, March 2022.
5. Discussion
This study is the first regional evaluation of readiness capacity described for cholera. The readiness status was assessed for countries and by pillars. This assessment based on expert opinion enabled consensual evaluation of the country capacity among the main cholera stakeholders. The approach of validating the tool content by using a panel of experts to assess its elements and rate them based on their relevance and representativeness has proven to be a rigorous method [13]. However, the results of the assessment for countries that had not reported cholera more than five years should be interpreted with caution as cholera may not be seen as major health emergency threat in these countries. As operational readiness requires, among others, political commitment, financing, human resources and equipment [14], countries where cholera is not or no longer major public health problems will not consequently prioritize it, especially in resources-limited settings.
5.1 About the Countries’ Readiness Level for Cholera in the Region
The overall countries’ readiness level to detect and respond to cholera was insufficient [15-16]. No country in this study had a good readiness capacity to early detect and respond to cholera outbreaks including in major hotspots. The readiness level reported is challenging especially for high-cholera burden countries where the occurrence of cholera is frequent and recurrent [2]. This can lead to delays in outbreaks detection and in response establishment as reported in previous outbreaks [17]. During the COVID-19 pandemic, there was a similar checklist developed to assess countries’ readiness level to early detect and respond to the disease. While no country was found to have good capacity for cholera, eight countries were assessed as adequately prepared for COVID-19 in February 2020 by the World Health Organization Regional Office for Africa [18]. Despite the novelty of COVID-19, the level of readiness was then higher than the cholera one. This is indicative of insufficient resources injected in cholera prevention and control despite its high burden. The level of the readiness reported can also be explained by insufficient implementation by Member States of the recommendation of the annual report on global preparedness for health emergencies in 2019. This report recommended that heads of government commit more to preparedness and build strong health systems. While the report highlighted that governments must prioritize and dedicate domestic resources and recurrent spending for preparedness as an integral part of national and global security, universal health coverage and the Sustainable Development Goals [19], funding is being the major issue in improving countries readiness to cholera. The readiness level varies from one country to another as well as per pillar [12] but overall, the readiness level was limited despite the fact that WHO African Member States are usually affected by cholera outbreaks with the very high magnitude outbreak reported in 2021 [2]. This raised the issues of insufficient implementation of lessons learned from previous outbreaks as well as the weak compliance with the preparedness requirements of GHS and IHR. During after action review on cholera outbreaks, it was commonly reported that delays in the outbreak detection led to high number of deaths reported at earlier stage of outbreaks; and recommendations to improve preparedness and readiness to next outbreaks are usually made. If efforts are being done in some countries, the hotspots analysis was recently conducted in some of them, and they are then not yet able to improve readiness capacities in at least 80% of the validated hotspots as required by the assessment tool. As mentioned above, countries’ overall readiness level was defined by the level of preparedness in each pillar. Among these pillars, the most concerning was the level of surveillance pillar. While surveillance is key for early detection and response to cholera outbreak [20], a proportion of 87% of assessed countries reported inadequate readiness level in surveillance including in community-based surveillance, training on the integrated disease surveillance and response (IDSR) and promptness [15,21]. The African Region is implementing IDSR for over decades, with capacity building in different settings. However, it seems that the strategy fails in availing needed capacities in major cholera hotspots. Efforts should be made to improve the number of districts with trained experts on IDSR. The WaSH and food safety pillar was also concerning. While weaknesses in WaSH are known as main predisposing factors of cholera outbreaks [3], just only one country reported good readiness capacity. This finding is in adequation with extended and protracted weaknesses reported in WaSH capacities across countries [22-24] due essentially to poor investment in basic infrastructure. The identification of hotspots must have been an opportunity for improving WaSH capacity by effectively prioritizing interventions to those in major needs in hotspots [3]. The case management readiness results were below the expected targets of the regional framework for the implementation of the global strategy for cholera prevention and control 2018 – 2030. There was no country with good readiness capacity in case management while this framework defined the year 2020 for countries to establish sufficient and specific capacity for cholera case management [4]. This can explain issues reported in case management with high CFR [2]. Laboratory appears as the most performing pillar across the region. Fifteen (15) countries had good or moderate readiness capacities in laboratory. This is linked with the strengthened capacity of national reference laboratory in organizing cholera confirmation in the Region. The reference laboratories across countries established functional mechanisms for samples collection and transport and preposition rapid diagnostic tests (RDT) in major hotspots.
5.2 About the added value of the assessment
The results of this assessment should be analyzed with caution for some countries. Countries like Madagascar did not report any cholera case in the past 20 years; other countries assessed did not also report cholera cases since 5 to 10 years. Cholera may not be seen as priority diseases for these countries, and this can explain the relatively low readiness level reported in these countries. However, this assessment is a kind of a reminder to these countries to keep cholera preparedness as part of their action plan for health security and ensure that minimum capacities for early detection and timely response are established. For countries at highest risk of cholera, this first comprehensive readiness assessment revealed weaknesses in early detecting and controlling cholera. These results bring to the stakeholders’ attention areas where major interventions should be oriented in order to improve countries’ readiness. The development of this assessment tool and its use are starting points of regular assessments of the countries’ readiness and close monitoring of progress in each pillar. This will enable to track progress in the health system capacity to deal with cholera threats and succeed in eliminating cholera by 2030. In fact, achieving readiness is a continuous process of establishing, strengthening, and maintaining a multisectoral response infrastructure that can be applied at all levels [11]. Regular further assessments will be conducted to monitor progress in each country and ensure that readiness of countries is improved and maintained. Building on the results of this first assessment and in order to improve the situation, a regional multi-countries readiness workshops are being conducted. Four sessions out of six are completed in Lomé, Togo; Niamey, Niger; Kinshasa, Democratic Republic of the Congo; and Nairobi, Kenya with participation of 160 multisectoral stakeholders from 18 countries (Benin, Burkina Faso, Burundi, Cameroon, Central Africa Republic, Chad, Congo, Côte d’Ivoire, The Democratic Republic of Congo, Ethiopia, Kenya, Mali, the Niger Republic, Senegal, South Sudan, Togo, Uganda and Zimbabwe). These trainings are aiming to provide capacities for early detection of cholera outbreaks, establishment of adequate response within the 48 first hours as well as ability to train multisectoral stakeholders in cholera hotspots. The results of the study were achieved. However, even though the assessment tool provided many insights into level of preparedness and capacity countries have to detect or respond to cholera outbreaks, there are some limitations. The weighting of pillars based on experts’ opinion can be debated [16]. The result of the assessment for a given country is dynamic and susceptible to change through improvement or deterioration. This is being overcome by follow-up assessments planned each six months. The self-assessment process can lead to over scoring of some criteria. But overall, these limitations did not affect the results and their implication for the countries readiness as the findings are in adequation with scientific and empiric findings across the region.
6. Conclusion
This cholera readiness assessment revealed insufficient capacities in countries for early detection and response to outbreaks. There was no country with adequate capacity in the Region. Nevertheless, seven countries had moderate capacity while sixteen had limited capacity. Laboratory pillar was the best performing area with eight countries having good capacity. Based on the findings of the study, cholera readiness capacity building workshops are being organized. The study provides each country with clear view on areas of improvements for better readiness for cholera. Regular assessments will be conducted to track progress.
Acknowledgments
We thank all Ministries of Health, Ministries of water and other lines ministries staff; country-specific partners and WHO staff involved in the assessment in all participating countries (Benin, Burkina Faso, Côte d’Ivoire, DRC, Ethiopia, Ghana, Kenya, Madagascar, Malawi, Mali, Mozambique, Namibia, The Niger Republic, Rwanda, Senegal, Sierra Leone, South Sudan, Tchad, Tanzania, Togo, Uganda, Zambia and Zimbabwe).
References
- Mboussou F, Ndumbi P, Ngom R et al. Infectious disease outbreaks in the African region: Overview of events reported to the World Health Organization in 2018. Epidemiology and Infection 147 (2019): 1-8.
- Sodjinou VD, Talisuna A, Braka F et al. The 2021 cholera outbreaks in West Africa: epidemiology and public health implications. Archives of Clinical and Biomedical Research 6 (2022): 296-307.
- Global task force on cholera control. Ending cholera: A global roadmap to 2030. 32 (2017).
- Regional Committee for Africa 68. Regional framework for the implementation of the global strategy for cholera prevention and control, 2018–2030. 1(2018).
- World Health Organization. Operational readiness and preparedness for Ebola virus disease outbreak in countries neighbouring the Democratic Republic of the Congo: progress, challenges and the way forward. Weekly Epidemiological Record 94 (2019): 39-43
- Norris SL, Sawin VI, Ferri M, et al. An evaluation of emergency guidelines issued by the World Health Organization in response to four infectious disease outbreaks. PLoS One 13 (2018): e0198125
- World Health Organization. Consolidated Ebola virus disease preparedness checklist -revised version 18 (2015).
- World Health Organization. Ebola virus disease preparedness strengthening team – Mali country visit report 2014. Geneva. World Health Organization 35 (2014).
- World Health Organization. Ebola virus disease preparedness strengthening team-Côte d’Ivoire country visit report 2014. Geneva. World Health Organization 30 (2014).
- World Health Organization. Ebola virus disease preparedness strengthening team – Mauritania country visit report 2014. Geneva. World Health Organization 24 (2014).
- Kandel M, Chungong S, Omaar A, et al. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. The lancet 395 (2020): 1047-1053.
- Heymann DL, Chen L, Takemi K, et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. The Lancet 395 (2015): 1884-1901.
- Almanasreh E, Moles R, Chen TF. Evaluation of methods used for estimating content validity. Research in social and administrative pharmacy 15 (2019): 214-221.
- World Health Organization. A strategic framework for emergency preparedness. 2017. Geneva. World Health Organization 29 (2017).
- Ateudjieu J, Yakum NM, Goura PA, et al. Health facility preparedness for cholera outbreak response in four cholera-prone districts in Cameroon: a cross sectional study. BMC Health Services Research 19 (2019): 458.
- Vong S, Samuel R, Gould P, et al. Assessment of Ebola virus disease preparedness in the WHO South-East Asia Region. Bulletin of the World Health Organization 94 (2016): 913.
- Elimian KO, Mezue S, Musah A, et al. What are the drivers of recurrent cholera transmission in Nigeria? Evidence from a scoping review. BMC Public Health 20 (2020): 432.
- Talisuna A, Nanyunja M, Stephen M, et al. COVID-19 pandemic preparedness and readiness in the WHO African Region: baseline status, best practices, lessons learnt, challenges and perspectives for the future. Weekly epidemiological report 96 (2021): xiv – xx.
- Global preparedness monitoring board. Un monde en péril : rapport annuel sur l’état de préparation mondial aux situations d’urgence sanitaire. Geneva. Global prepraedness monitoring goal 48 (2019).
- Spiegel PB, Ratnayak R, Hellman N, et al. Cholera in Yemen: a case study of epidemic preparedness and response. 2018. Baltimore. Johns Hopkins Center for Humanitarian Health 108 (2018).
- Sparrow A, Almilaji K, Tajaldin B, et al. Cholera in the time of war: implications of weak surveillance in Syria for the WHO’s preparedness—a comparison of two monitoring systems. BMJ Global Health 1 (2016): e000029.
- Elimian KO, Musah A, Ochu CL, et al. Identifying and quantifying the factors associated with cholera-related death during the 2018 outbreak in Nigeria. Pan Afr Med J 37 (2020): 368.
- Visa T, Emmanuel T, Mbodi F, et al. Risk factors associated with cholera outbreak in Mubi Adamawa state – Nigeria, 2018. International Journal of Infectious Diseases 101 (2020): 266.
- Gallandat K, Jeandron A, Ross I, et al. The impact of improved water supply on cholera and diarrhoeal diseases in Uvira, Democratic Republic of the Congo: a protocol for a pragmatic stepped-wedge cluster randomised trial and economic evaluation. Trials 22 (2021): 408.