A Substitute of Ultrasound Acoustic Stand-Off Pad Made From Locally Available Material: An innovation to Survive in Resource Limited Conditions
Article Information
Sandeep Moudgil1, Lokesh Singh2,*, Sunil Raina3
1Assistant Professor, Department of Radio diagnosis, IGMC Shimla, India
2Research Associate, Department of Radio diagnosis, PGIMER Chandigarh, India
3Professor and Head, Department of Community Medicine, RPGMC Tanda Kangra, HP, India
*Corresponding author: Lokesh Singh, Research Associate, Department of Radio diagnosis, PGIMER, Chandigarh, India
Received: 30 November 2020; Accepted: 08 December 2020; Published: 12 January 2021
Citation: Sandeep Moudgil, Lokesh Singh, Sunil Raina. A Substitute of Ultrasound Acoustic Stand-Off Pad Made From Locally Available Material: An innovation to Survive In Resource Limited Conditions. Archives of Clinical and Biomedical Research 5 (2021): 61-67.
Share at FacebookAbstract
Introduction: The use of stand-off acoustic pads for ultrasonographic evaluation of the superficial structures is well established. These are costly and not available readily at peripheral and remote community level institutes like ours. This instigated to make a simple and cheaper substitute to these stand-off pads. A cost effective alternative for these commercial acoustic stand-off pads made by using locally available condom and ultrasound jelly is presented here.
Material and Methods: A latex condom, commonly available in hospital supplies, was filled with ultrasound coupling jelly. All the air was removed and a knot was secured at the end. The coupling jelly was applied between the skin condom and condom transducer interface while scanning. Superficial lesion of different body regions, breast and superficial foreign bodies were evaluated using the condom stand off pads.
Observations: Scanning the area of interest using condom stand-off pad showed the overlying skin details, depth of lesion from the skin, internal architecture of the lesion and surrounding tissue in more detail than scanning without pad. The image quality of breast tissue or lesions located just below the nipple in sub retro-areolar region was better than these areas of interest scanning without pad. It also aided in evaluating the depth of superficial foreign body from the skin surface which helped in their surgical or image guided retrieval.
Conclusion: The material used in making these condom stand-off pads is easily available and very cheap. The condom stand-off described here will help the radiologists working in remote or rural areas by providing them an easy to make and cheaper substitute in a resource limited setting. The quality of image and ease to handle is not as that of commercially available stand-off pads nevertheless condom stand-off pads
Keywords
Stand-off pads; Acoustic stand-off pads; Condom stand-off pad; Uses of condom
Stand-off pads articles; Acoustic stand-off pads articles; Condom stand-off pad articles; Uses of condom articles
Article Details
1. Introduction
Stand-off pads aid in imaging superficial lesions, lesions involving or located immediately below the skin, superficial foreign bodies and in imaging breast lesions [1-3]. Stand-off pads increases the distance between the ultrasound transducer and a superficially located lesions and brings the area of interest with in the transducer focal zone. It removes or reduces the reverberations in area of interest and improves image quality [2]. Improved image quality helps to evaluate the skin involvement, internal details of the lesion and size, exact depth of the lesion from the skin surface especially when lesion is larger than the field of view of the transducer placed directly over the skin [1, 3].
Commercially available stand-off pads are costly and are of limited availability [4]. Both of these factors are of concern for a radiologist practicing radiology at peripheral and remote areas where the nearest availability of commercial pad is approximately 150-200 kilometers, that too in a hilly terrain. This further adds to delay or cause suboptimal scans. With this background a simple and cheaper substitute for these commercially available stand-off pads was made.
We contrived a cheaper condom stand-off using locally available material at our peripheral level community hospital i.e. using a condom and ultrasound jelly, which were available in hospital supply and offered a very cheap (no direct cost) and readily available solution. It is sonolucent, hypoallergic, firm and provides adequate area for foot of the probe and serves the purpose fairly well almost at par to their commercial counterparts after a little practice. The entire condom pad or coupling jelly used for filling can be reused.
2. Technique
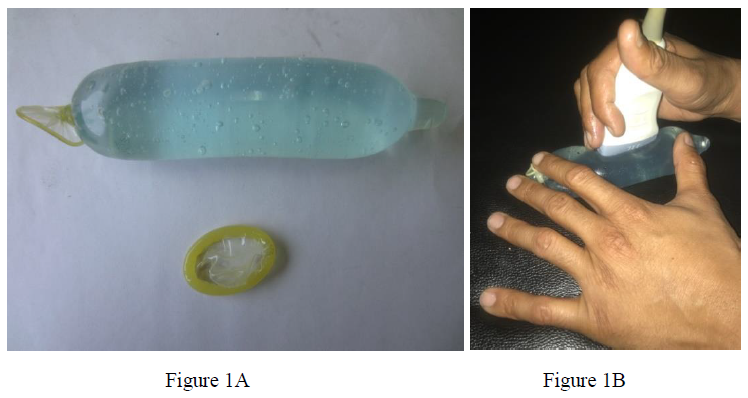
A latex condom that was available in hospital supply (costing approximately 3-5 Indian rupees ~0.05 USD, over the counter) was filled with ultrasound coupling jelly and end was secured with a knot. Care was taken to keep the air trapping to the minimum while filling the jelly and securing the knot. The condom was filled up to two third of its capacity with the final unit measuring approximately 6-10 cm which is enough to accommodate the foot of the linear probe, (Figure 1A-B).
‘Stand-off’ pad was then placed over the area of interest and scanning was done applying the coupling jelly between the skin-condom and condom-transducer interfaces. The pad can be stabilized with one hand while holding the probe in other, (Figure 1B). This technique requires an assistant to operate the machine controls. Probe and pad can be held simultaneously using the same hand. A little practice is needed to hold the cylindrical shape of the condom stand-off pad and probe using the fingers of the same hand simultaneously but has a short and steep learning curve. Care should be taken not to press the pad too hard with the probe as higher pressure displaces the jelly to the sides leaving no ‘stand-off’ effect while scanning.
3. Observations
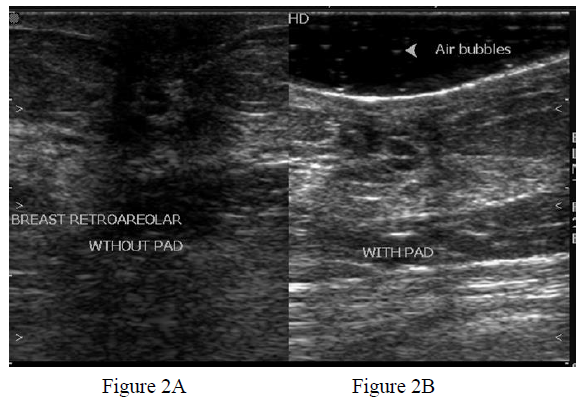
This condom stand-off pad was used to evaluate various superficial lesions of different regions of the body. It has shown to serve the purpose fairly well as mentioned in the literature on the commercially available acoustic stand-off pads. While evaluating breast abscesses or other breast lesions depth and the skin overlying the lesion (Figure 2B) was better visualized than scanning without acoustic pad (Figure 2A). As expected, more details of the sub/retro-areolar area or lesion were available on scanning with pad than scanning without stand-off pad (Figure 2A and Figure 2B).
Figure 2: Gray scale ultrasound image of breast using a linear high frequency transducer without (Figure 2A) and with (Figure 2B) condom stand-off pad. Details of the lesion i.e. dilated ducts in sub/retro areolar region are better seen in Figure 2B. Tiny air artefacts are also seen (arrowhead Figure 2B) causing no significant deterioration of image quality. The skin and depth of the dilated ducts are shown well while using the pad (Figure 2B).
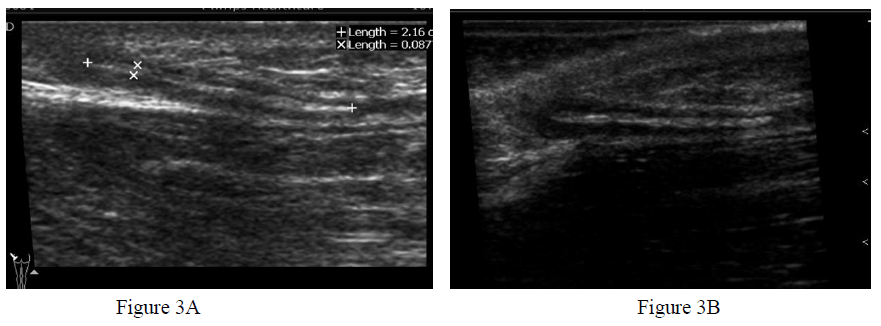
Figure 3: Wooden foreign body in gluteal region evaluated without (Figure 3A) and with (Figure 3B) stand-off pad. The overlying skin and distance of the superficial end from the skin are well shown while using the pad (Figure 3B) which helps in planning the guided retrieval of the foreign body. The peripheral hypoechoic rim which suggests the inflammatory reaction and raises the possibility of the wooden foreign body is clearly demonstrated while using the pad (thin arrow in Figure 3B, as compared with Figure 3A).
By using the pad, exact depth of the foreign body from the skin could be measured (Figure 3B), which was not possible while evaluating without stand-off pad, (Figure 3A), since transducer foot is in direct contact with skin. Knowledge of the depth from and status of the superficial skin helps in planning the image guided retrieval of these foreign bodies. Since using the pad offers better details, this may aid in suggesting the possible nature of the foreign body (as in Figure 3B, a clear hypoechoic peripheral rim indicative of inflammatory reaction is seen raising possibility of wooden foreign body).
4. Discussion
Various materials and techniques have been described and tried to keep the probe off the skin surface aiding the ultrasonographic evaluation of superficial structures or pathologies affecting skin, subcutaneous areas, breast lesions or superficial foreign bodies. Acoustic-pads are mentioned of help in evaluating the superficial breast lesion by American College of Radiology [5]. Water filled glove finger, water bath (for limbs) a thick layer of jelly or various commercially available stand-off pads have been described widely for evaluating superficial lesions [6].
Water filled glove finger is helpful in evaluating smaller lesions but its size limits the larger lesion evaluation. Water bath technique also offers similar advantage but cannot be used to evaluate the larger body parts (like gluteal area in Figure 3B), [6]. Ideal stand-off pad should be sonolucent, hypoallergic, firm, cheap and readily available and should have adequate area to accommodate the probe foot.
Commercially available pads, though meet these criterions well but are costly (especially in countries like ours where an ultrasonographic scan at state owned institutes costs approximately USD 2-4 while commercially available pads are of minimum of USD 5 or more!) [4]. Cost is big consideration in resource limited areas like ours, as well as the availability of these products.
The availability and procurement of such logistics may not be feasible especially at smaller rural or community level health care centers as ours is another issue as commercial pads are available in the main cities, which are usually 150-200 kilometers away.
A condom stand-off pad presented here, was made from locally available material and is very cheap, easy to prepare and can be reused after washing with soap and water or hand sanitizers, if needed. The material required to prepare is readily available even at very primary level health institute, and hence, can be made any time anywhere by using a very simple technique described here.
We used these condom stand-off pads were used to evaluate superficial lesions like those of breast, thyroid, gluteal regions, face hand and wrist etc. These were also useful in evaluating superficial foreign bodies, added confidence to establishing the diagnosis, aided in evaluating and measuring exact depth from skin surface (Figure 3B) and in their image guided retrieval.
These ‘condom contraption’ have limitations too. Multiple tiny air bubbles may get trapped if due care is not taken while filling the jelly into the condom, which may interfere while imaging, deteriorating the image quality. This can be reduced significantly by simply warming the jelly in hot water bath before pouring into condom. Warming makes the jelly less viscid and more free flowing hence becomes easy to pour into the condom reducing the chances of air entrapment.
Some experience is required to handle these pads as they are more cylindrical and tend to slip away during examination. We used little/ring finger and thumb of the left hand to fix both ends of the pad over the area of interest and scanned by holding the probe with other hand (two hand technique, Figure 1B). Even same hand can be used to hold the probe between thumb and index finger and other fingers and base of thumb to fix the pad. Probe should be held very gently against the pad as excessive pressure on the probe may displace the jelly away, making the probe to lie in direct contact with skin resulting in loss of ‘acoustic stand-off’ effect.
The overall image quality produced is acceptable as the air bubbles are very tiny and do not cause too dirty shadowing to deteriorate the image quality.
Making and using these condom stand-off pads has a short and steep learning curve and the image deterioration due bubbles in jelly or unsteadiness in handling the probe become insignificant (Figure 2B, minimal tiny air bubbles causing no significant image deterioration) with time and a good acoustic stand-off effect is produced. These can be used after sterilizing with commonly available hospital hand sanitizers. Commercially available stand-off pads a still better in handling and the image quality produced but these also serve the purpose well enough.
5. Conclusion
Stand-off pads aid in evaluation of superficial lesions but commercial stand-pads are costly and are of limited availability. These factors are of concern especially at peripheral level and remote institutes where the resources are limited. The condom stand-off described here is a cheaper substitute that can be made from readily available material in a resource limited setting and help the radiologist working in remote or rural areas. As expected, the quality of image and ease to handle is less than commercially available stand-off pads nevertheless it serves the purpose fairly well and are reusable. Image quality and ease to handle improves as user gains experience in preparing and handling these condom stand-off pads.
Conflicts of Interest
Nil.
Funding
Nil.
References
- Stavros AT. Breast Ultrasound, Philadelphia: Lippincott Williams and Wilkins (2004): 21-22.
- Biller DS, Myer W. Ultrasound Scanning of Superficial Structures Using an Ultrasound Standoff Pad. Veterinary Radiology 29 (1998): 138-142.
- Fornage BD, Schernberg FL. Sonographic diagnosis of foreign bodies of the distal extremities. American Journal of Roentgenology 147 (1986): 567-569.
- https://www.amazon.com/Parker-Labs-Aquaflex-Ultrasound%20Pads/dp/B002R2SP2Y
- http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/US_Breast.pdf
- Jeong HY, Krishnamurthy R. 1012: Water-Bath Method for Sonographic Evaluation of Superficial Structures of the Extremities. Ultrasound in Medicine and Biology 35: S101-S102.