A Study on Duplex Doppler Ultrasonography as a Non-Invasive Test for Diagnosis of Portal Hypertension in Children Attending a Tertiary Care Hospital in Bangladesh
Article Information
Marjan P1*, Karim ASMB2, Rukunuzzaman M3, Das SR4, Mondal M5, Sarker N6, Akther H7, Nahar L8, Chowdhury AS9
1Junior Consultant (Paediatrics), Labaid Specialized Hospital, Dhaka, Bangladesh
2Professor and Chairman (Ex), Department of Pediatric Gastroenterology and Nutrition, BSMMU, Dhaka, Bangladesh
3Professor and Chairman, Department of Pediatric Gastroenterology and Nutrition, BSMMU, Dhaka, Bangladesh
4Medical Officer, Department of Pediatric Gastroenterology and Nutrition, BSMMU, Dhaka, Bangladesh
5Medical Officer, Upazila Health Complex, Munshiganj, Bangladesh
6Assistant Professor (Paediatrics), Bangabandhu Sheikh Mujib Medical College, Faridpur, Bangladesh
7Medical Officer, Upazila Health Complex, Shariatpur, Bangladesh
8Registrar (Pediatric Gastroenterology), Dhaka Medical College Hospital, Dhaka, Bangladesh
9Junior Consultant, Department of Paediatrics and NICU, Labaid Specialized Hospital, Dhaka, Bangladesh
*Corresponding Author: Parisa Marjan, Junior Consultant (Paediatrics), Labaid Specialized Hospital, Dhaka, Bangladesh
Received: 11 January 2022; Accepted: 17 January 2022; Published: 21 January 2022
Citation:
Marjan P, Karim ASMB, Rukunuzzaman M, Das SR, Mondal M, Sarker N, Akther H, Nahar L, Chowdhury AS. A Study on Duplex Doppler Ultrasonography as a Non-Invasive Test for Diagnosis of Portal Hypertension in Children Attending a Tertiary Care Hospital in Bangladesh. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 083-093.
Share at FacebookAbstract
Background: Portal hypertension is the hemodynamic abnormality frequently associated with serious liver disease, although it is recognized in a variety of extrahepatic diseases also. Endoscopy of upper GIT is the gold standard for diagnosis of oesophageal varices but it is invasive, costly and not easily available. Doppler ultrasound is a non-invasive, relatively cheap and easily accessible imaging modality that helps in making the diagnosis of clinically significant portal hypertension.
Objective: To observe the efficacy of Doppler Ultrasonography for predicting the presence of portal hypertension in children.
Methods: This cross-sectional descriptive study was conducted at the Department of Pediatric Gastroenterology & Nutrition, BSMMU during the period Jan 2018 to July 2019. 47 patients who were diagnosed as portal hypertension by upper GIT endoscopy were selected purposively according to inclusion and exclusion criteria. Demographic data and other related information regarding etiology and complications were recorded in a standard datasheet. Doppler USG was done in Nuclear medicine department, BSMMU by a single sonologist. Collected data were checked manually and analyzed by computer-based program SPSS for Windows (version 22.0).
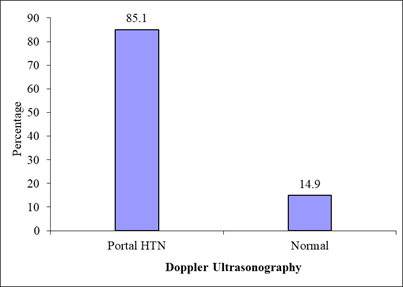
Results: 47 patients were enrolled in this study with a mean age of 9.2 ± 3.9 years. 42.6% of patients were diagnosed as CLD and 57.4 % were extrahepatic portal hypertension. Among CLD patients Wilson disease was the most common etiology (61%). Doppler USG could detect portal hypertension in 85% of patients. Among 3 different parameters (Portal vein parameter, portal vein flow velocity, the direction of flow in portal vein) of Doppler USG, portal vein flow velocity was most sensitive in detecting portal hypertension. PV: BSA was superior to portal vein diameter alone for diagnosing portal hypertension (p < 0.05). When endos
Keywords
Duplex Doppler Ultrasonography, Portal Hypertension, PV Diameter, CLD
Duplex Doppler Ultrasonography articles; Portal Hypertension articles; PV Diameter articles; CLD articles
Article Details
1. Introduction
Portal hypertension is the hemodynamic abnormality frequently associated with serious liver disease, although it is recognized in a variety of extrahepatic diseases also. Portal hypertension (PHTN) and bleed-ing from oesophageal varices in children remain a difficult medical problem [1]. The gold standard for the diagnosis of portal hypertension is direct measurement of portal pressure or hepatic venous pressure gradient [2]. These measurements can be obtained only by invasive methods, which are not feasible in most centers of the world. The indirect way to assess PHTN is by detection of oesophageal varices. There are a number of ways to assess the status of oesophageal varices, these are barium swallow of oesophagus, ultrasonography and upper gastrointestinal endoscopy. The search for a non-invasive biochemical or imaging marker for the sev-erity (stage) and/or etiology of chronic liver disease (CLD) in adults, as well as children, is needed nowadays. Real time ultrasonography (US) has become an integral part of the non-invasive evalu-ation of the liver in many clinical settings in adults [3]. But there are few studies regarding the efficacy of Doppler USG as a non-invasive test for diagnosing portal hypertension in children. In this point of view, this study is aimed to determine whether Doppler Ultrasonography is effective to determine presence and severity of portal hypertension.
2. Materials and Methods
This cross-sectional descriptive study was conducted at the Department of Pediatric Gastroenterology & Nutrition, BSMMU during the period Jan 2018 to July 2019. 47 patients who were diagnosed as portal hypertension by upper GIT endoscopy were selected purposively according to inclusion and exclusion criteria.
2.1 Inclusion criteria
1. The patients below 18 years of age diagnosed as portal hypertension.
2.2 Exclusion criteria
- Active or recent (within 2 weeks) upper GI bleeding.
- Patient on beta blocker therapy.
- Endoscopic sclerotherapy or band ligation done for esophageal varices.
- Previous surgery for portal hypertension.
Demographic data and other related information regarding etiology and complications were recorded in a standard datasheet. Written informed consent was taken from the parent. Endoscopy of upper GIT to detect oesophageal varices and other required investigations to detect etiology and complications were carried out as required after admission. Doppler USG was done in Nuclear medicine department, BSMMU by a single sonologist. Collected data were checked manually and analyzed by computer-based program SPSS for Windows (version 22.0). Several parameters (portal vein diameter, PV: BSA, mean portal vein flow velocity, flow direction, and cavernous transformation) were considered to evaluate the effectiveness of Doppler USG to detect portal hypertension. Comparison of parameters among themselves to detect varices was done by Z test of proportion and the usefulness of them to differentiate between etiology and association with endoscopic grading of varices was done using a chi-square test of independence. P values <0.05 was considered as significant.
3. Results
Total 47 children who were diagnosed as portal hypertension by endoscopy of upper GIT were analyzed in this study. It was observed that 20 (42.6%) patients belonged to age group 6-10 years. The mean age was 9.22 ± 3.85 years with ranged from 1.5 to 16 years. Male children were 29 (67.7%). Among 47 patients 27 were diagnosed as extrahepatic portal hypertension and 20 were diagnosed as CLD with portal HTN.
|
Etiology of portal HTN |
No of patients |
Percentage of patient |
|
Extra hepatic portal HTN |
27 |
57.4% |
|
Wilson disease |
12 |
25.5% |
|
Budd chiari syndrome |
2 |
4.3% |
|
Chronic Hep B |
1 |
2.12% |
|
Biliary cirrhosis |
1 |
2.12% |
|
Histoplasmosis |
1 |
2.12% |
|
Cryptogenic |
2 |
4.3% |
|
Autoimmune hepatitis |
1 |
2.12% |
Table 1: Etiology of Portal Hypertension (N=47).
|
Endoscopy of upper GIT |
No of patients |
percentage |
|
Esophageal varices |
||
|
Grade 1 |
3 |
6.4% |
|
Grade 2 |
14 |
29.8% |
|
Grade 3 |
11 |
23.4% |
|
Grade 4 |
19 |
40.4% |
|
Fundic varices |
||
|
Yes |
7 |
14.9% |
|
No |
40 |
85.1% |
|
Gastropathy |
||
|
Yes |
3 |
6.4% |
|
No |
44 |
93.6% |
Table 2: Endoscopic findings of studied patients (N=47).
|
Doppler USG findings |
No of patients |
Percentage |
|
Coarse liver parenchyma |
||
|
Present |
36 |
76.6% |
|
Absent |
11 |
23.4% |
|
Splenomegaly |
||
|
Present |
46 |
97.9% |
|
Absent |
1 |
2.1% |
|
Cavernous transformation |
||
|
Present |
14 |
29.8% |
|
Absent |
33 |
70.2% |
|
Portal vein diameter |
||
|
< 13 mm |
42 |
97.7% |
|
>13 mm |
1 |
2.3% |
|
PV flow velocity (cm/sec) |
||
|
>13 |
15 |
31.9% |
|
≤13 |
32 |
68.4% |
|
Direction of flow |
||
|
Hepatopetal |
38 |
80.9% |
|
Hepatofugal |
9 |
19.1% |
Table 3: Doppler Ultrasonographic findings of studied patients (N=47).
|
USG parameter |
Portal HTN |
p value |
|||
|
Absent |
Present |
||||
|
n |
% |
n |
% |
||
|
*PV diameter(mm) (n=43) |
42 |
97.7 |
1 |
2.3 |
<0.001 |
|
PV flow velocity (cm/s) n= 47 |
15 |
31.9 |
32 |
68.1 |
|
*PV diameter of 4 patients could not be evaluated
Table 4: Association of diagnosis with PV diameter and PV flow velocity.
|
USG parameter |
Portal HTN |
p value |
|||
|
Absent |
Present |
||||
|
n |
% |
n |
% |
||
|
PV flow velocity (cm/s) n= 47 |
15 |
31.9 |
32 |
68.1 |
0.001 |
|
Direction of flow |
38 |
80.9 |
9 |
19.1 |
|
Table 5: Association of diagnosis with PV flow velocity and direction of blood flow (N=47).
|
Diagnosis |
*PV diameter (n=43) |
PV: BSA (n=43) |
p value |
||
|
N |
% |
N |
% |
||
|
Normal |
42 |
97.7 |
34 |
79.1 |
0.007 |
|
Portal HTN |
1 |
2.3 |
9 |
20.9 |
|
Table 6: Comparison between PV diameter and PV: BSA for as diagnostic parameter of portal hypertension (n=47).
|
Esophageal varices |
PV flow velocity (cm/sec) |
p value |
|||||
|
Mild(9-13) n=21 |
moderate(6-9) n=5 |
severe(3-6) n=5 |
0.127 |
||||
|
N |
% |
N |
% |
N |
% |
||
|
Small (1-2) |
8 |
38.1 |
0 |
0.0 |
3 |
60.0 |
|
|
Large (3-4) |
13 |
61.9 |
5 |
100.0 |
2 |
40.0 |
|
Table 7: Comparison between endoscopic grading and Doppler classification of portal hypertension (n=47).
Table 1 shows the etiology of portal hypertension of studied patients. Extrahepatic portal hypertension was the most common etiology (57.4%). Among CLD patients Wilson disease was the most common (12; 25.5%). Two (4.3%) patients were cryptogenic CLD and two (4.3%) were Budd Chiari Syndrome. One patient was Biliary cirrhosis and one patient had Auto immune hepatitis. Table 2 shows the distri-bution of the studied patients by endoscopy of upper GIT. It was observed that 19 (40.4%) patients had Grade-4. Seven (14.9%) patients had fundic varices. Three (6.4%) patients had gastropathy. Table 3 shows the distribution of the studied patients by ultrasonographic findings. It was observed that more than one thirds (76.6%) patients had liver coarse echotexture. Majority (97.9%) patients had spleen-omegaly. Almost one third (29.8%) patients had cavernous transformation. Majority (97.7%) patients belonged to PV diameter <13. More than two third (68.1%) patients belonged to PV flow velocity ≤13 m/sec2. Majority (80.9%) patients had hepatopedal blood flow. Only 19% had hepatofugal flow. Table 4 was observed that 1(2.3%) patients were diagnosed as portal HTN by assessing PV diameter (>13mm), 32(68.1%) by portal vein flow velocity (< 13cm/sec) and 9(19.1%) by direction of blood flow (hepatofugal). In table 5 comparison between PV diameter and PV flow velocity for diagnosing portal HTN was shown (p< 0.001). In table 4 comparison between portal vein flow velocity and direction of flow was assessed for diagnosing portal HTN (P=0.001). So overall decreased PV flow velocity was superior to other parameters for diagnosing portal HTN. Table 6 shows was observed that 1 (2.3%) patient was diagnosed as portal hypertension by PV diameter (>13mm) and 9 (20.9%) patients were diagnosed as portal hypertension by PV: BSA (>12). The difference was statistically significant (p<0.05). Table 7 shows the comparison between endoscopic grading and Doppler classification of varices .It was observed that almost two thirds (61.9%) patients with large esophagus varices diagnosed as mild (9-13), 5(100.0) as moderate (6-9) and 2 (40.0%) as severe (3-6) by assessing portal vein flow velocity in Doppler USG. The difference was statistically not significant (p>0.05).
3.1 Diagnosis of portal hypertension by dopper USG
Figure1 shows 40 (85%) patients were diagnosed as portal hypertension by Doppler USG whenone or more doppler parameters were taken in consideration including PV diameter, PV flow velocity, direction of flow and cavernous transformation.
4. Discussion
Portal hypertension is the hemodynamic abnormality frequently associated with serious liver disease, although it is recognized in a variety of extrahepatic diseases [4]. It is estimated that approximately 50% of pediatric patients with chronic liver disease and 90% of those with extrahepatic portal vein obstruction (EHPVO) will experience gastrointestinal bleeding [5]. Oesophago-gastro-duodenoscopy is required to detect the gastro oesophageal varices. But the procedure is invasive, painful to the patient and is not available in all centres. Whereas portal vein diameter can be measured by an easily available, painless, and noninvasive method like ultraso-nography (USG) [6]. Doppler ultrasound is a non-invasive, relatively cheap and easily acssessible imaging modality that helps in making the diagnosis of clinically significant portal hypertension [7]. A total of 47 patients with portal hypertension were included in this study. Their ages were between 1.5 to 16 years. Most (42%) of the patients were in the age group between 6-10 years.
The mean (±SD) age of the studied patients was found to be 9.2 ± 3.85years, male was 61% and female 38%. Similar results were also observed in another study done in Bangladesh [8]. Karim et al (1999). In his study 31 (56%) were male and 24 (44%) female. In another study done in BSMMU [9]. Hussain et al.[9] patient's age group was found between 2 to 15 years and male female ratio was 4:1. In this study the most common etiology of portal hypertension was extrahepatic (57%), 2 seperate studies done on Indian children showed that 76.5% and 54% cases of portal hypertension were extra-hepatic. Arora et al.[10] Podder et al.[11] Mahmud et al. (2015) .Another study done in bangladesh 40 children with portal hypertension and found 32 (80%) due to pre-hepatic causes and 08 (20%) due to hepatic causes.. Most common etiology of chronic liver disease was found to be Wilson disease (12; 60%).Another study done at BSMMU found similar result alam et al [12]. The predominant etiology of CLD was Wilson’s disease (n=55, 65.5%). Infective hepatitis was the most common cause of CLD in a study done in Shishu Hospital Alam et al [13]. It was observed that the pattern of etiology is regionally variable. In our region extrahepatic is the most cammon cause of portal hypertension. Regarding etiology of CLD we found Wilson disease was the commonest cause. But as our institution is the tertiary care centre it may not reflect the scenario of In this study, upper GIT endoscopy showed 47 (100%) patients had oesophageal varices. 3 (6.4%) cases had grade I, 14 (29.8%) cases had grade II, 11 (23.4%) cases grade III, and 19 (40.4%) cases had grade IV oesophageal varices. Gastric varices in particular, pose a common and difficult problem with an estimated prevalence of between 17 and 20% in patients with portal hypertension. Fagundes et al. [14] found gastric varices in 19% cases. In the present study it was found in 14.9% cases. Portal hyprtensive gastropathy was seen only in 6.4 % cases whereas in another study gastropathy was diagnosed in 58.8% cases [15].
In Doppler USG splenomegaly was found in 97.9% cases. Lafortune et al [16] found splenomegaly in 80% cases. Portal vein dilatation was found in only one patient (2.3%). But in a study done on adult patients. Chakenahalli et al. [17] dilated portal vein was noted in 39 of 58 cases (67.2%). Diameter of portal vein could not be measured in 5 cases where portal vein was not delineated due to cavernoma formation. In this study also in 4 patients diameter could not be measured due to cavernoma. Portal vein dilatation > 13 mm may be a feature of portal hypertension in adults but not in children. Riahinezhad et al [18] found portal vein diameter increased in patients with oesophageal varices in comparison to healthy control but it was not > 13mm. It was shown that portal vein diameter strongly varies with age and anthropometric variables like height, weight and chest circumference [19]. Lafortune et al. [16] found in their study that dilated portal vein was not diagnostic of portal hypertension. Koslin et al. [20] found portal vein diameter alone was not sufficient for diagnosis of portal hypertension. In this study portal vein diameter was compared to PV: BSA for diagnosing portal hypertension. PV: BSA ratio was found superior to diameter alone (p < 0.05). Giacomo et al [21] showed in a study that portal vein diameter is age dependant in case of children and not differed in portal HTN and control patients. They showed PV: BSA >12 is a reliable marker for diagnosing portal hypertension in children. As portal vein diameter in children depends on age and antropometry so instead of portal vein diameter alone we should consider PV: BSA for diagnosis of portal hypertension in children. Hepatofugal flow (flow directed away from the liver) is abnormal in any segment of the portal venous system. The most common cause of hepatofugal flow in the portal venous system is portal hypertension.
The prevalence of hepatofugal flow in the portal venous system in studies of patients with cirrhosis evaluated with Doppler USG varies between 3% and 23% [22]. Lafortune et al [16] found hepatofugal flow is an absolute sign of potal hypertension with a sensitivity of 85% and specificity 100%. In our study only 9 (19%) had hepatofugal flow which is similar to study by Mittal et al [23] where six patients (12%) among a total of fifty had non hepatopetal flow (hepatofugal/bidirectional). Gaiani et al [24] found only 3.1% patients of portal hypertension had hepatofugal flow. Another study showed reversal of blood flow is a sign of advanced portal hypertension [25]. So it may not be found in all cases of portal hypertension unless patient has advanced disease. The portal vein mean velocity was significantly lower in cirrhotic children with esophageal varices than those without varices [18]. In our study most of the patients had low mean portal vein velocity. In extrahepatic portal hypertension portal vein obstruction by thrombus or cavernoma may be the cause of decreased portal vein flow velocity [26]. We considered 13 cm/sec as the cut off for diagnosing portal hypertension (as per Indian childhood classification). But in many studies 15 cm/sec was the cut off value for diagnosis. Gianni et al. [24] found the value of 15 cm/s was considered the best cut-off value, showing a sensitivity and specificity of 88% and 96%, respectively. When the doppler parameters were compared portal vein flow velocity was found superior in diagnosing portal hypertension (p <0.05). But according to grading of portal hypertension by mean portal vein velocity it could not detect the severity of portal hypertension. Gorka et al [27] found similar result in their study. In that study portal vein flow velocity was lower in patients with varices but it did not correlate with the severity of varices. Haang et al [28] also stated that Dupplex sonography contributes to the diagnosis of portal hypertension but did not assess its grading. But study done by El-Shabrawi et al [3] showed in children with cirrhosis that portal flow velocity might be correlated with the severity of portal hypertension. Kozaiwa et al [29] also showed patient with lowest portal vein velocity had oesophageal varices and gastric varices with red color sign. As we included both CLD and extrahepatic portal hypertension it might be the cause that we did not find any correlation with the severity of varices.
5. Conclusion
Doppler USG can be used as a non-invasive test for diagnosis of portal hypertension in children. In case children PV: BSA> 12 can be used as a marker for diagnosis of portal hypertension in spite of PV diameter alone. Portal vein flow velocity is a very good marker for diagnosing portal hypertension. In brief, Doppler US examination may provide bene-ficial information on evaluating children with this may guide the paediatricians in descision making in terms of further evaluation, prophylactic management and prevention of life threatening complications.
References
- Carale J. Portal Hypertension. Medscape (2017).
- Sherlock S, Doolly J, Anna L, et al. Sherlock’s Diseases of liver and Biliary System, 12th ed, Blackwell Publishing Ltd, London (2012): 152-233.
- El-Shabrawi MHF, El-Raziky M, Sheiba M, et al. Value of duplex doppler ultrasonography in non-invasive assessment of children with chronic liver disease. World Journal of Gastroenterology 6 (2010): 6139-6144.
- Keerthi K, Kumar HVS, Karla VB. Doppler A very helpful diagnostic tool for evaluating portal hypertension. Journal of Evidence based Medicine and Helthcare 2 (2015): 2397-2401.
- Adami RM, Ferreire CT, Kieling OC, et al. Noninvasive methods for prediction of esophageal varices in pedicatric patients with portal hypertension. World Journal Gastroenterology 19 (2013): 2053-2069.
- Mandal L, Mandal SK, Bandyopadhay D, et al. Correlation of portal vein diameter and splenic size withgastro-oesophageal varices in cirrhosis of liver’, Journal, Indian Academy of Clinical Medicine 12 (2015): 266-270.
- Anand A, Sonawane B, Gupta S, et al. Portal Hypertension Evaluation by Doppler Ultrasound ’, IOSR Journal of Dental and Medical Sciences 13 (2014): 25-28.
- Karim ASMB, Akter S, Karim MA, A study of clinical profile of chronic liver disease in children. Dhaka Shishu Hospital Journal 15 (1999): 15-72.
- Hussain F, Karim ASMB, Matin MA, et al. Portal Hypertension:2 years’ Experience in Department of Pediatric Gastroenterology and Nutrition, at a Tertiary Care Hospital, Bangladesh’, Journal of Shaheed Suhrawardy Medical College 8 (2016): 26-29.
- Arora NK, Lodha R, Gulati S, et al. Portal hypertension in North Indian Children. Indian Journal of Pediatrics 65 (1998): 585-591.
- Podder U, Thapa BR, Rao KL, et al. Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West?’, Journal of Gastroenterology and Hepatology 23 (2008): 1354-1357.
- Alam R, Karim ASMB, Rukunuzzaman M, et al. Non-endoscopic predictors of esophageal varices in children with chronic liver disease and their utility in resource-constrained countries. Indian Journal of Gastroenterology (2019).
- Alam MJ, Ahmed F, Mobarak R, et al. Pattern of liver diseases in children admitted in Dhaka Shishu Hospital. International Journal of Hepatology 1 (2010): 18-24.
- Fagundes EDT, Perreira A, Roquete MLV, et al. Clinical and Labroatry Predictors of Esophageal Varices in children and Adolescents with portal hypertension Syndrom. Journal of Pediatric Gastroenterology and Nutrition 46 (2008): 178-183.
- Aydogoan A, Gulluoglu M, Onder SY, et al. Portal Gastropathy and Duodenopathy in Children with Extrahepatic and Intrahepatic Portal Hypertension: Endoscopic Diagnosis and Histologic Secoring. Journal of Pediatric Gastroentenrology and Nutrition 52 (2011): 612-616.
- Lafortune M, Marleau D, Breton G, et al. Portal Venous System Measurements in Portal Hypertension. Radiology 151 (1984): 27-30.
- Chakenahalli N, Narasipur R, Varun, et al. Role of Ultrasound Doppler in Evaluation of Portal Hypertension. International Journal of Anatomy, Radiology and Surgery 7 (2018): 5-10.
- Riahinezhad M, Rezaei M, Saneian H, et al. Doppler assessment of children with liver cirrhosis and portal hypertension in comparison with a healthy control group: An analytical cross-sectional study. Journal of Research in Medical Sciences 23 (2018): 40.
- Ghosh T, Banarjee M, Basu S, et al. Assesment of normal portal vein diameter. Tropical Gastroenterology 35 (2014): 79- 84.
- Koslin DB, Mulligan SA, Berland LL. Duplex assessment of the portal venous system. Seminars in Ultrasound, CT and MRI 13 (1992): 22-33.
- Giacomo CD, Tomasi G, Gatti C, et al. Ultrasonographic prediction of the presence and severity of oesophageal varices in children. Journal of Pediatric Gastroenterology and Nutrition 9 (1989): 431-435.
- Wachsberg RH, Bahramipour P, Sofocleous CT, et al. Hepatofugal flow in the Portal Venous System: Pathophysiology, Imaging Findings, and Diagnostic Pitfalls. Radiographics 22 (2002): 123-140.
- Mittal P, Gupta R, Mittal G, et al. Association Between Portal Vein Color Doppler Findings and the Severity of Disease in Cirrhotic Patients With Portal Hypertension. Iranian Journal of Radiology 8 (2011): 211-217.
- Gaiani S, Bolondi L, Li Bassi S, et al. Prevalence of spontaneous hepatofugal portal flow in liver eirrhosis. Clinical and endoscopic correlation in 228 patients. Gastroenterology 100 (1991): 160-167.
- Kondo T, Maruyama H, Sekimoto T, et al. Reversed portal flow: Clinical influence on the long-term outcomes in cirrhosis. World Journal of Gastroenterology 21 (2015): 8894-8902.
- Pargewar SS, Desai SN, Rajesh S, et al. Imaging and radiological interventions in extra-hepatic portal vein obstruction. World Journal of Radiology 8 (2016): 556-570.
- Gorka W, Al Mulla A, Al Sebayel M. Qualitative hepatic venous Doppler sonography versus portal flowmetry in predicting the severity of esophageal varices in hepatitis C cirrhosis Children. American Journal of Roentology 169 (1997): 511-515.
- Haag K, Roessle M, Ochs A. Correlation of duplex Doppler sonography findings and portal pressure in 375 patients with portal hypertension. Americam Journal of Roentology 172 (1998): 631-635.
- Kozaiwa K, Tajiri H, Yoshimura N, et al. Utility of Duplex Doppler Ultrasound in Evaluating Portal Hypertension. Jaurnal of Pediatric Gastroenterology and Nutrition 201 (1995): 215-219.