A Report on Prenatal Diagnosis of a Rare Case of Fetal Acrania and Omphalocele by Doppler Examination
Article Information
Sabar Butt1*, Syeda Khadija1, Syed Amir Gilani2
1Department of Radiological Sciences and Medical Imaging Technology, University of Lahore, Lahore, Pakistan
2Faculty of Allied Health Sciences, University of Lahore, Lahore, Pakistan
*Corresponding Author: Sabar Butt, Sabiry ultrasound training institute, 411-A Ghulam Muhammad Abad, Faisalabad
Received: 03 December 2019; Accepted: 24 December 2019; Published: 15 January 2020
Citation: Sabar Butt, Syeda Khadija, Syed Amir Gilani. A report on prenatal diagnosis of a rare case of fetal acrania and omphalocele by Doppler examination. Journal of Radiology and Clinical Imaging 3 (2020): 003-012.
Share at FacebookAbstract
A congenital anomaly, fetal acrania (exencephaly) is, in which the fetal brain is not surrounded completely or partially by the skull bones. It is suggested that there is lacking of mesenchymal migration in the fourth week of embryological age. The first-trimester diagnosis must be made with restraint because the fetal cranium is not fully calcified before 10-11 weeks; therefore, if only midsagittal views of the fetus are obtained, misdiagnosis may occur. Another anomaly, omphalocele, a ventral defect of the umbilical ring resulting in herniation of the abdominal viscera, is one of the most common congenital abdominal wall defects seen in the newborn. Omphalocele is associated with trisomy [18]. The defect occurs in 1 in 6000 to 1 in 10,000 live births. The anencephaly sequence begins with acrania, which affecting the central nervous system with an incidence of ~1:1000 pregnancies. In our case a female 28 years old visited our ultrasound clinic for anomaly scan. The gestational age was 18 weeks 4 days. On ultrasound examination the presentation of fetus was cephalic and longitudinal lie. The sonographic scan revealed fully developed fetal brain having no calvarium. The brain was covered by a thin membranous structure. Compression of fetal brain by transducer was observed due to absence of cranium. The scan revealed the brain floating in the amniotic fluid over the base of skull. Facial structures were normal. Normal and well-coordinated movements were noted in in the fetal body parts. There was symmetry in Fetal nose and naso-labial folds and were well appreciated. It was also noted that spinal canal showed normal morphology with normal Cervical, thoracic and lumbar spines. The fetal abdomen showed a central mass protruding out from anterior abdominal wall. The mass is covered by a membrane and contains small intestines and liver. There was direct insertion of the umbilical cord into the midline of omphalocele. After taking consent form
Keywords
Ultrasonography; Omphalocele; Acrania; Doppler ultrasound
Ultrasonography articles, Omphalocele articles, Acrania articles, Doppler ultrasound articles
Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals Omphalocele articles Omphalocele Research articles Omphalocele review articles Omphalocele PubMed articles Omphalocele PubMed Central articles Omphalocele 2023 articles Omphalocele 2024 articles Omphalocele Scopus articles Omphalocele impact factor journals Omphalocele Scopus journals Omphalocele PubMed journals Omphalocele medical journals Omphalocele free journals Omphalocele best journals Omphalocele top journals Omphalocele free medical journals Omphalocele famous journals Omphalocele Google Scholar indexed journals Acrania articles Acrania Research articles Acrania review articles Acrania PubMed articles Acrania PubMed Central articles Acrania 2023 articles Acrania 2024 articles Acrania Scopus articles Acrania impact factor journals Acrania Scopus journals Acrania PubMed journals Acrania medical journals Acrania free journals Acrania best journals Acrania top journals Acrania free medical journals Acrania famous journals Acrania Google Scholar indexed journals Doppler ultrasound articles Doppler ultrasound Research articles Doppler ultrasound review articles Doppler ultrasound PubMed articles Doppler ultrasound PubMed Central articles Doppler ultrasound 2023 articles Doppler ultrasound 2024 articles Doppler ultrasound Scopus articles Doppler ultrasound impact factor journals Doppler ultrasound Scopus journals Doppler ultrasound PubMed journals Doppler ultrasound medical journals Doppler ultrasound free journals Doppler ultrasound best journals Doppler ultrasound top journals Doppler ultrasound free medical journals Doppler ultrasound famous journals Doppler ultrasound Google Scholar indexed journals exencephaly articles exencephaly Research articles exencephaly review articles exencephaly PubMed articles exencephaly PubMed Central articles exencephaly 2023 articles exencephaly 2024 articles exencephaly Scopus articles exencephaly impact factor journals exencephaly Scopus journals exencephaly PubMed journals exencephaly medical journals exencephaly free journals exencephaly best journals exencephaly top journals exencephaly free medical journals exencephaly famous journals exencephaly Google Scholar indexed journals sonographic scan articles sonographic scan Research articles sonographic scan review articles sonographic scan PubMed articles sonographic scan PubMed Central articles sonographic scan 2023 articles sonographic scan 2024 articles sonographic scan Scopus articles sonographic scan impact factor journals sonographic scan Scopus journals sonographic scan PubMed journals sonographic scan medical journals sonographic scan free journals sonographic scan best journals sonographic scan top journals sonographic scan free medical journals sonographic scan famous journals sonographic scan Google Scholar indexed journals lumbar spines articles lumbar spines Research articles lumbar spines review articles lumbar spines PubMed articles lumbar spines PubMed Central articles lumbar spines 2023 articles lumbar spines 2024 articles lumbar spines Scopus articles lumbar spines impact factor journals lumbar spines Scopus journals lumbar spines PubMed journals lumbar spines medical journals lumbar spines free journals lumbar spines best journals lumbar spines top journals lumbar spines free medical journals lumbar spines famous journals lumbar spines Google Scholar indexed journals umbilical cord articles umbilical cord Research articles umbilical cord review articles umbilical cord PubMed articles umbilical cord PubMed Central articles umbilical cord 2023 articles umbilical cord 2024 articles umbilical cord Scopus articles umbilical cord impact factor journals umbilical cord Scopus journals umbilical cord PubMed journals umbilical cord medical journals umbilical cord free journals umbilical cord best journals umbilical cord top journals umbilical cord free medical journals umbilical cord famous journals umbilical cord Google Scholar indexed journals amorphous brain mass articles amorphous brain mass Research articles amorphous brain mass review articles amorphous brain mass PubMed articles amorphous brain mass PubMed Central articles amorphous brain mass 2023 articles amorphous brain mass 2024 articles amorphous brain mass Scopus articles amorphous brain mass impact factor journals amorphous brain mass Scopus journals amorphous brain mass PubMed journals amorphous brain mass medical journals amorphous brain mass free journals amorphous brain mass best journals amorphous brain mass top journals amorphous brain mass free medical journals amorphous brain mass famous journals amorphous brain mass Google Scholar indexed journals microphthalmia articles microphthalmia Research articles microphthalmia review articles microphthalmia PubMed articles microphthalmia PubMed Central articles microphthalmia 2023 articles microphthalmia 2024 articles microphthalmia Scopus articles microphthalmia impact factor journals microphthalmia Scopus journals microphthalmia PubMed journals microphthalmia medical journals microphthalmia free journals microphthalmia best journals microphthalmia top journals microphthalmia free medical journals microphthalmia famous journals microphthalmia Google Scholar indexed journals
Article Details
1. Introduction
A midline abdominal wall defect of variable size,called Omphalocoele is covered by a membrane of amnion and peritoneum with Wharton’s jelly between the two layers, and enclosing abdominal contents. The defect occurs at the base of the umbilical cord, with the cord/umbilical vessels inserting at the apex of the omphalocele sac [1]. Acrania anencephaly sequence is the progression from a relatively normal-appearing exposed brain due to an absent cranium (acrania) to an amorphous brain mass (exencephaly) to no recognisable brain tissue (anencephaly). Lack of mesenchymal migration in the fourth week of embryological age is a proposed mechanism. Fetal acrania can be diagnosed from 11 weeks onward. At 11-14 weeks gestation, the majority of cranial ossification is in the lateral aspects of the frontal bones and lower parietal bones, and no vault ossification is visible in the midline on a perfect mid sagittal image. Severe Osteogenesis imperfecta and congenital hypophosphatasia result in poor mineralization of the calvarium. In these cases sonography may demonstrate poorly defined calvaria which can be conceivably difficult to differentiate from acrania [2]. The incidence of isolated fetal omphalocele was estimated as 1:2165 (0.046%) [3, 4]. The detection rate and accurate rate of fetal omphalocele were 100 % and 100% respectively. The recurrence risk for an isolated omphalocele in a subsequent pregnancy is < 1% [5]. The incidence of omphalocele around the world is estimated as 1 in every 3000-5000 fetuses [6]. The acrania, anencephaly sequence begins with acrania, which affecting the central nervous system with an incidence of ~1:1000 pregnancies [7].
2. Case Presentation
A 28 years old female was referred to our ultrasound clinic for anomaly scan. The gestational age was 18 weeks 4 days. The mother had urban background and was not well aware about antenatal checkup she could not recall her 1st day of menstrual cycle and expected date of delivery. She was not enrolled and no previous record. Her alpha-fetoprotein level was not measured. On ultrasound examination the presentation of fetus was cephalic and longitudinal lie. The sonographic scan revealed fully developed fetal brain having no calvarium (acrania) (Figure1 and 2). Outer surface of the brain (cerebral cortex) was much 'wrinkled' (convoluted), inter-hemispheric fissure and sulci were well identified. The brain was covered by a thin membranous structure (Figure 3). Compression of fetal brain by transducer was observed due to absence of cranium. The brain was floating in the amniotic fluid over the base of skull (Figure3). Facial structures were normal. The fetus showed normal cardiac activity (137 beats /min) with normal rhythm. The fetal body parts showed normal and well-coordinated movements. Placenta was anterior with normal thickness (Figure 4). Both orbits were symmetrical in size and shape. Fetal nose and naso-labial folds were appreciated and seemed symmetrical (Figure 3 and 4). Cervical, thoracic and lumbar spines appeared normal with normal morphology of the spinal canal. Fetal long bones were normal (Figure 3). The fetal abdomen showed a central mass protruding out from anterior abdominal wall. The mass is covered by a membrane and contains small intestines and liver. (Figure 6a and 6b) There was direct insertion of the umbilical cord into the midline of omphalocele, which was confirmed by Doppler. (Figure 7a and 7b) after taking consent form from the patient and her family, an elective prostaglindin abortion was performed. After delivery placenta was completely removed. Aborted fetal examination revealed lack of fetal cranium (Figure 6). Fetal facial features were normal. Brain was covered by a membrane. There was a mass protruding through anterior abdominal wall and multiple abdominal visceras were protruding out through the midline gap in the anterior abdominal wall (Figure 7). This breach was centrally located equivalent to umbilicus connection. About 1-2mm thick membrane was covering the protruding organs. The parents did not allow for post- partum examination. This discontinuation in midline corresponding to the umbilical area with acrania without family history is indicative of central omphalocoele which can be easily discriminated from correspondingly presenting right Para median anomaly known as gastroschisis.
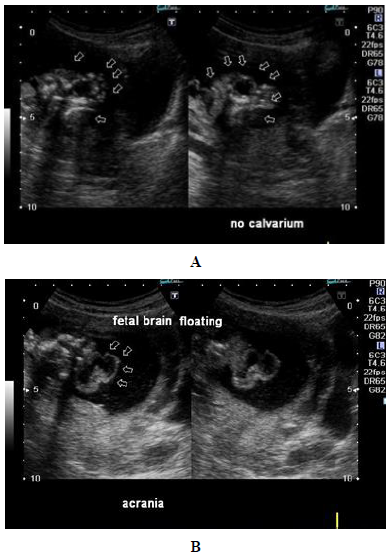
Figure 1: (a) Fetal Acrania. Gray scale ultrasound of the fetal brain (T4.6 MHz probe) in axial plane. Gestational age 18 weeks 4 days. No skull is seen around the brain (arrows). Arrowhead=amniotic fluid around the brain. Asterisk indicates inter-hemispheric fissure; (b) Fetal Acrania. Gray scale ultrasound of the fetal brain (T4.6 MHz probe) in coronal plane. Gestational age 18 weeks 4 days. No skull is seen around the brain (arrows).
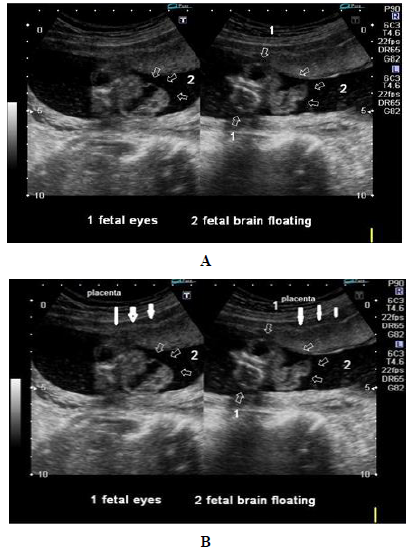
Figure 2: (a) Fetal Acrania. Gray scale ultrasound of the fetal brain in coronal plane. Gestational age 18 weeks 4 days. The brain floating in the amniotic fluid over the base of skull; (b) Fetal Acrania. (A) Gray scale ultrasound of the fetus in sagittal plane. Gestational age 18 weeks 4 days. Arrows = The brain was floating in the amniotic fluid over the base of skull. Both orbits were symmetrical in size and shape. Fetal nose and naso-labial folds were appreciated and seemed symmetrical (Figure 3). White Arrows= Placental position anterior and normal thickness.

Figure 3: Fetal Acrania and omphalocoele . (A) Gray scale ultrasound of the fetus (T4.6 MHz probe) in sagittal plane. Gestational age 18 weeks 4 days. Normal fetal long bone.
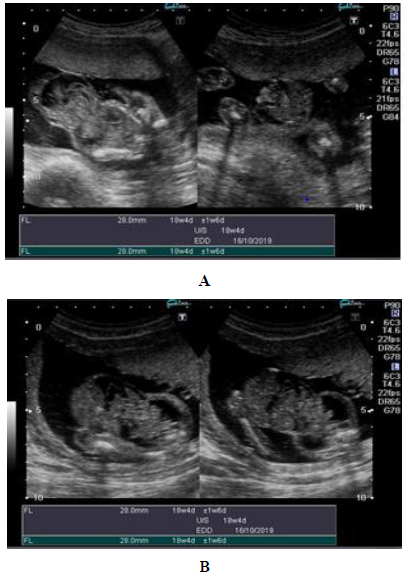
Figure 4: Fetal Acrania and omphalocoele . (A) Gray scale ultrasound of the fetus (T4.6 MHz probe) in sagittal showing central mass protruding out from anterior abdominal wall. The mass is covered by a membrane and contains small intestines and liver.
ne.
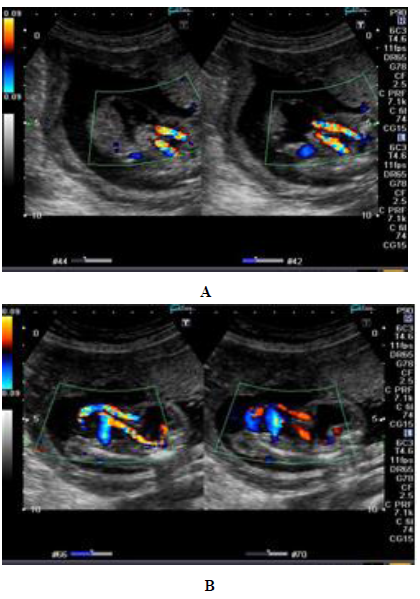
Figure 5: Color Doppler ultrasound showing direct insertion of the umbilical cord into the midline of omphalocele. (Figure 5a and 5b).

Figure 6: Aborted fetus showing lack of fetal cranium, Fetal facial features normal. Brain was covered by a membrane. The mass protruding through anterior abdominal wall.

Figure 7: Aborted fetus showing normal nose, facial parts, normal musculature and limbs.
3. Discussion
Omphalocele is a result of abnormal closure or absence of midline anterior abdominal wall which results in extrusion of abdominal viscera. They are routinely subdivided into epigastric, central, and infra-umbilical omphalocele regarding the location of breach, commonest is the central [8]. Previous Studies exhibits strong correlation of the central type of defect with an abnormal karyotype (69%) of which trisomy 18 was most frequently noted [9]. Little numbers of patients with such defect were associated with good prognosis (8%) [8]. The pathological causes of omphalocele and gastroschisis are questionable and have multiple theories regarding origin [14]. Occurrence of omphalocele (1 in 4000) is rare than gastroschisis (1 in 2000) [10]. Deng et. al, after reading 827 cases of omphalocele from the year 1996 to 2006, established that 52.4% of pregnancies ended with late fetal death with upward trend in successive years and 37.4% resulted in early neonatal death [9]. Our case is rare because of incidence of non-isolated omphalocele (27.9%) was very less compared to isolated cases (72.1%) verifying the lesser incidence of syndromic feature of the defect [9]. The patients in the gestational age of 28-36 weeks had mortality rate 2.42 times higher than 37-42 weeks and therefore earlier diagnosis will help us proper management of more cases well within time [11]. Other anomalies which occur with omphalocele are cleft palate and spinal deformity, but some less common anomalies have been reported as well. Findings of a rare syndrome of caudal regression introduced by Duhamel characterized by continuum of anorectal, urogenital and skeletal congenital abnormalities, imperforate anus and presence of congenital idiopathic clubfoot was somewhat parallel to our case [12]. If we compare other investigations, assessment of fetal structure and well-being by ultrasound is most trustworthy but the lack in the proper examination and infrequent routine checkups lead to a large proportion of undiagnosed cases. In the health centers only about 39.3% of cases are being diagnosed and the rest 60.6% are established by physical examination after birth similar to our report [13]. This evidence supported our concern towards the lack of awareness and proper diagnosis as projected in our report. Acrania is a rare developmental anomaly, a type of neural tube defects in which there is partial or complete absence of cranial bones although there is complete development of brain tissue [14]. In exencephaly, which is congenital anomaly, there is disorganized brain tissue in a large amount extending from the abnormal skull [15]. Epithelium is covering the brain tissue and can get rapid necrosis due to amniotic fluid and become small and degenerate to the anencephaly [16]. The exencephaly is a rare congenital anomaly that occurs in the spectrum of the acrania and anencephaly [17]. Neural tube defects is caused by many factors .In studies, Genetic transition was detected when NTD seen with a syndrome. In most of the cases karyotyoing is normal. Therefore no family history in the acrania-exencephaly, so chromosomal analysis is not recommended. The threat of reappearance of NTD increase 10-20 times who have previously in NTD birth stories? Researches proved that NTD is commonly seen whose feeds are deficient of zinc and folic acid [18]. Formerly, the cases of anencephaly diagnosed in the 2nd trimester is identified in the early pregnancy period due to the 1st trimester screening test being between 11th and 14th week [19]. The cranial bones ossification starts from the 10thweek of gestation and this ossification is noticeable in the ultrasound from the 11th week [20]. In the literature 9-week 3-days acrania was reported. But maximum of the reported cases are at the earliest in 10-14 weeks of gestation [21]. Ultrasonographic findings of first trimester exencephaly; decreased size of the cranial region compared to the chest, irregularity of cranial surface, and amniotic fluid echogenicity. Calvarial bones were not observed in the first trimester ultrasonography of our case but ompholocele and normal brain tissue were observed [22]. The case we are reporting, there is coexistence of the two may be part of some specific syndromes. Other abnormalities can accompained to the acrania-exencephaly-anencephaly such as neural tube defects, omphalocel, liver and heart anomalies, cleft palate-lip, microphthalmia etc., [18, 19]. In this case, we present acrania with accompanying omphalocele. It might be a genetic transition, but the family did not approve genetic research. Our case revealed that early diagnosis of congenital cranial anomalies is possible by ultrasonography such as exencephalia. It is also evident that it can be together with other congenital anomalies and therefore should not be missed. Congenital anomaly like exencephaly and also acrania-anencephaly in this spectrum have lethal reasons and also additional abnormalities can be accompanying such as omphalocele as in this case report. Therefore, careful ultrasonographic examination prenatally can easily diagnose and such cases will enable early termination with consent of family.
4. Conclusion
Omphalocele is a rare congenital anterior abdominal wall abnormality effecting infant mortality and quality of life. Fetal acrania is a rare and lethal congenital anomaly that warrants the identification of fetal skull and cranium around the brain that should be normally calcified. The diagnosis of such defect is necessary to be made well within time. Approach with better strategies to either electively terminate the pregnancy or assess the viability of fetus should be made followed by implementation of the optimal treatment protocol. The fact about lacking awareness and proper diagnosis yearns for more efficient training of health practitioner, proper reporting, and increased availability of diagnostic tools such as advanced ultrasonographic examination and availability of genetic screening in several neglected regions of developing country.
5. Recommendations
Ultrasonography is a helpful examination for early detection of omphalocele and acrania, but further studies on large scale should be done, especially in endemic areas. After the prenatal diagnosis of fetal omphalocele, the parents received genetic consultations to decide whether to continue pregnancy or termination at our hospital or other clinics. Karyotyping should also be performed by amniocentesis or cord blood sampling. Autopsy should be undertaken for selective cases after the family gave informed consent.
Source of Support
Nil.
Conflict of Interest
None.
References
- Prasad S, Paragannavar L. Acrania: a case report. Science and Technology 13 (2015): 5.
- Li L, Cerda S, Kindelberger D, et al. Isolated Acrania in the Presence of Amniotic Band Syndrome. North American Journal of Medicine and Science 10 (2017): 101.
- Cincore V, Ninios AP, Pavlik J, et al. Prenatal diagnosis of acrania associated with amniotic band syndrome. Obstetrics & Gynecology 102 (2003): 1176-78.
- Cheng CC, Lee FK, Lin HW, et al. Diagnosis of fetal acrania during the first trimester nuchal translucency screening for Down syndrome. International Journal of Gynecology and Obstetrics 80 (2003): 139-44.
- Pajkrt E, Van Lith JM, Mol BW, et l. Screening for Down's syndrome by fetal nuchal translucency measurement in a general obstetric population. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology 12 (1998): 163-169.
- Smith NM, Chambers HM, Furness ME, et al. The OEIS complex (omphalocele-exstrophy-imperforate anus-spinal defects): recurrence in sibs. Journal of medical genetics 29 (1992): 730-732.
- Fong KW, Toi A, Salem S, et al. Detection of fetal structural abnormalities with US during early pregnancy. Radiographics 24 (2004):157-174.
- Brantberg A, Blaas HG, Salvesen KÅ, et al. OC064a: Poor outcome of fetuses with omphaloceles. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology 22 (2003): 17.
- Deng K, Qiu J, Dai L, et al. Perinatal mortality in pregnancies with omphalocele: data from the Chinese national birth defects monitoring network. BMC pediatrics 14 (2014): 160.
- Gupta U, Tiwari P, Kumari R, et al. A report on omphalocele and associated congenital deformity with intrauterine death: Need for early diagnosis. International Journal of Students’ Research 5 (2015): 34.
- Sadler TW. The embryologic origin of ventral body wall defects. In Seminars in pediatric surgery 19 (2010): 209-214.
- Agarwal R. Prenatal diagnosis of anterior abdominal wall defects: Pictorial essay. Indian Journal of Radiology and Imaging 15 (2005): 361.
- Liang YL, Kang L, Tsai PY, et al. Prenatal diagnosis of fetal omphalocele by ultrasound: a comparison of two centuries. Taiwanese Journal of Obstetrics and Gynecology 52 (2013): 258-263.
- Cox GG, Rosenthal SJ, Holsapple JW. Exencephaly: sonographic findings and radiologic-pathologic correlation. Radiology 155 (1985): 755-756.
- Visser ’t Hooft M, Peters N, Ursem N, et al.Primary or delayed omphalocele closure prediction in the second trimester of pregnancy. Ultrasound in Obstetrics & Gynecology Wiley 38 (2011): 162.
- Cullen MT, Green J, Whetham J, et al. Transvaginal ultrasonographic detection of congenital anomalies in the first trimester. American journal of obstetrics and gynecology 163 (1990): 466-476.
- Becker R, Mende B, Stiemer B, et al. Sonographic markers of exencephaly at 9+ 3 weeks of gestation. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology 16 (2000): 582-584.
- Bianca S, Ingegnosi C, Auditore S, et al. Prenatal and postnatal findings of acrania. Archives of gynecology and obstetrics 271 (2005): 257-259.
- Stoll C, Alembik Y, Dott B, et al. Omphalocele and gastroschisis and associated malformations. American journal of medical genetics Part A 146 (2008): 1280-1285.
- Frolov P, Alali J, Klein MD. Clinical risk factors for gastroschisis and omphalocele in humans: a review of the literature. Pediatric surgery international 26 (2010): 1135-1148.
- Di Tanna GL, Rosano A, Mastroiacovo P. Prevalence of gastroschisis at birth: retrospective study. BMJ: British Medical Journal 325 (2002):1389.
- Moore CA, Harmon JP, Padilla LM, et al. Neural tube defects and omphalocele in trisomy 18. Clinical genetics 34 (1988): 98-103.
