A Rare Case of Anti-N-Methyl-D-Aspartate Receptor Encephalitis with Status Epilepticus in Pregnancy
Article Information
Meryl M Sperling1*, Anne Waldrop1, Cedar Fowler2, Julianna J Weiel3, Charlotte L Conturie1, Katherine Bianco1
1Department of Obstetrics and Gynecology, Stanford University School of Medicine, Stanford, California, USA
2Department of Anesthesia, Stanford University School of Medicine, Stanford, California, USA
3Department of Pathology, Stanford University School of Medicine, Stanford, California, USA
*Corresponding Author: Meryl M Sperling, Department of Obstetrics and Gynecology, Center for Academic Medicine, MC 5317, Stanford University School of Medicine, 453 Quarry Road, Palo Alto, CA 94303, USA
Received: 13 May 2021; Accepted: 21 May 2021; Published: 31 May 2021
Citation:
Meryl M Sperling, Anne Waldrop, Cedar Fowler, Julianna J Weiel, Charlotte L Conturie, Katherine Bianco. A Rare Case of Anti-N-Methyl-D-Aspartate Receptor Encephalitis with Status Epilepticus in Pregnancy. Obstetrics and Gynecology Research 4 (2021): 108-116.
Share at FacebookAbstract
Background: Anti-N-methyl-D-aspartate (NMDA) receptor encephalitis is an autoimmune disorder that can lead to psychosis and severe neurological symptoms and is extremely rare in pregnancy. It is often associated with an ovarian teratoma, with many having symptomatic improvement after its removal. Many patients have a prolonged recovery time to their baseline neurological status.
Case: This is a 33 year old G4P2012 who presented at 14 weeks gestation in status epilepticus after a 1 week history of acute behavioral changes, who was found to have an ovarian teratoma with anti-NMDA receptor encephalitis. She remained hospitalized throughout the duration of her pregnancy, which was complicated by drug induced hepatotoxicity, severe short term memory loss, tracheostomy and percutaneous gastric tube placement. The fetus was in breech presentation at 39 weeks, at which time an external cephalic version (ECV) was attempted and was unsuccessful, leading to an emergent primary cesarean delivery without complications.
Conclusion: Anti-NDMA receptor encephalitis is a rare event that can occur in pregnancy that can lead to debilitating neurological symptoms. Due to the complexity of these patients, optimal care should be focused around a multidisciplinary team in order to optimize maternal care. We did not find a need to deliver the patient preterm and followed standard obstetric management in guiding decision-making around her pregnancy.
Keywords
Anti-N-Methyl-D-Aspartate Receptor Encephalitis, Seizures, Teratoma, Dermoid, Status Epilepticus
Anti-N-Methyl-D-Aspartate Receptor Encephalitis articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis Research articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis review articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis PubMed articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis PubMed Central articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis 2023 articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis 2024 articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis Scopus articles Anti-N-Methyl-D-Aspartate Receptor Encephalitis impact factor journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis Scopus journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis PubMed journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis medical journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis free journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis best journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis top journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis free medical journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis famous journals Anti-N-Methyl-D-Aspartate Receptor Encephalitis Google Scholar indexed journals Seizures articles Seizures Research articles Seizures review articles Seizures PubMed articles Seizures PubMed Central articles Seizures 2023 articles Seizures 2024 articles Seizures Scopus articles Seizures impact factor journals Seizures Scopus journals Seizures PubMed journals Seizures medical journals Seizures free journals Seizures best journals Seizures top journals Seizures free medical journals Seizures famous journals Seizures Google Scholar indexed journals Teratoma articles Teratoma Research articles Teratoma review articles Teratoma PubMed articles Teratoma PubMed Central articles Teratoma 2023 articles Teratoma 2024 articles Teratoma Scopus articles Teratoma impact factor journals Teratoma Scopus journals Teratoma PubMed journals Teratoma medical journals Teratoma free journals Teratoma best journals Teratoma top journals Teratoma free medical journals Teratoma famous journals Teratoma Google Scholar indexed journals Dermoid articles Dermoid Research articles Dermoid review articles Dermoid PubMed articles Dermoid PubMed Central articles Dermoid 2023 articles Dermoid 2024 articles Dermoid Scopus articles Dermoid impact factor journals Dermoid Scopus journals Dermoid PubMed journals Dermoid medical journals Dermoid free journals Dermoid best journals Dermoid top journals Dermoid free medical journals Dermoid famous journals Dermoid Google Scholar indexed journals Status Epilepticus articles Status Epilepticus Research articles Status Epilepticus review articles Status Epilepticus PubMed articles Status Epilepticus PubMed Central articles Status Epilepticus 2023 articles Status Epilepticus 2024 articles Status Epilepticus Scopus articles Status Epilepticus impact factor journals Status Epilepticus Scopus journals Status Epilepticus PubMed journals Status Epilepticus medical journals Status Epilepticus free journals Status Epilepticus best journals Status Epilepticus top journals Status Epilepticus free medical journals Status Epilepticus famous journals Status Epilepticus Google Scholar indexed journals ovarian teratoma articles ovarian teratoma Research articles ovarian teratoma review articles ovarian teratoma PubMed articles ovarian teratoma PubMed Central articles ovarian teratoma 2023 articles ovarian teratoma 2024 articles ovarian teratoma Scopus articles ovarian teratoma impact factor journals ovarian teratoma Scopus journals ovarian teratoma PubMed journals ovarian teratoma medical journals ovarian teratoma free journals ovarian teratoma best journals ovarian teratoma top journals ovarian teratoma free medical journals ovarian teratoma famous journals ovarian teratoma Google Scholar indexed journals encephalopathy articles encephalopathy Research articles encephalopathy review articles encephalopathy PubMed articles encephalopathy PubMed Central articles encephalopathy 2023 articles encephalopathy 2024 articles encephalopathy Scopus articles encephalopathy impact factor journals encephalopathy Scopus journals encephalopathy PubMed journals encephalopathy medical journals encephalopathy free journals encephalopathy best journals encephalopathy top journals encephalopathy free medical journals encephalopathy famous journals encephalopathy Google Scholar indexed journals intrauterine pregnancy articles intrauterine pregnancy Research articles intrauterine pregnancy review articles intrauterine pregnancy PubMed articles intrauterine pregnancy PubMed Central articles intrauterine pregnancy 2023 articles intrauterine pregnancy 2024 articles intrauterine pregnancy Scopus articles intrauterine pregnancy impact factor journals intrauterine pregnancy Scopus journals intrauterine pregnancy PubMed journals intrauterine pregnancy medical journals intrauterine pregnancy free journals intrauterine pregnancy best journals intrauterine pregnancy top journals intrauterine pregnancy free medical journals intrauterine pregnancy famous journals intrauterine pregnancy Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals Maternal-fetal medicine articles Maternal-fetal medicine Research articles Maternal-fetal medicine review articles Maternal-fetal medicine PubMed articles Maternal-fetal medicine PubMed Central articles Maternal-fetal medicine 2023 articles Maternal-fetal medicine 2024 articles Maternal-fetal medicine Scopus articles Maternal-fetal medicine impact factor journals Maternal-fetal medicine Scopus journals Maternal-fetal medicine PubMed journals Maternal-fetal medicine medical journals Maternal-fetal medicine free journals Maternal-fetal medicine best journals Maternal-fetal medicine top journals Maternal-fetal medicine free medical journals Maternal-fetal medicine famous journals Maternal-fetal medicine Google Scholar indexed journals
Article Details
1. Introduction
Anti-NMDA receptor encephalitis has been described as an autoimmune process, often with a paraneoplastic immune response to a tumor, and it is the most common cause of non-viral encephalitis. It usually presents with progressive psychosis, seizures, and autonomic dysfunction [1]. In general, affected patients are young (mean age 23 years old), predominantly female, with approximately 60% of patients having an ovarian teratoma [2]. Treatment options include tumor removal, corticosteroids, intravenous immunoglobulin (IVIG), plasma exchange, and, less often, a cytotoxic agent such as rituximab or cyclophosphamide [3]. Within 24 months of treatment, 79% of patients demonstrate a return to their baseline function [4]. Anti-NMDA receptor encephalitis is a rare disease with only a few associated case reports in pregnancy. We present a case of a pregnant patient who was diagnosed with anti-NMDA receptor encephalitis early in pregnancy and who required hospitalization until delivery. The patient had a difficult hospital course that required multiple surgeries and management by a complex multi-disciplinary team. She ultimately delivered a healthy term neonate and continues to recover neurologically from her disease process 6 months after delivery.
2. Case Presentation
A 33 year old previously healthy G4P2012 initially presented at 14w1d after a witnessed seizure and a 1 week history of headache and odd behaviors (uncontrolled laughing, head banging against the wall, emotional lability, short-term memory loss, insomnia, and poor oral intake). She was transferred to our institution for a higher level of care after requiring intubation for airway protection in the setting of continued encephalopathy and ongoing, uncontrolled seizure activity. Evaluation at the outside hospital was notable for a lumbar puncture (LP) with lymphocytic pleocytosis (WBC 35/µL), but an otherwise negative infectious workup (appendix I and II). A computed tomography (CT) of the head and magnetic resonance imaging (MRI) of the brain were unremarkable. Multiple electroencephalograms (EEGs) performed prior to transfer demonstrated left temporal discharges and left focal status epilepticus (appendix III). On transfer, she was awake but unable to follow commands. For her anti-epileptic drugs (AEDs) she was continued on levetiracetam and phenytoin. Fosphenytoin, and valproate were also utilized. After transfer, repeat LP showed persistent lymphocytic pleocytosis and new findings of an increased opening pressure of 33 mm H2O (appendix I). Initial differential diagnosis included a high suspicion for autoimmune encephalitis vs herpes simplex virus (HSV) or other viral encephalitis vs less likely a primary seizure disorder given her presenting age.
A pelvic ultrasound was performed upon transfer, confirming a viable intrauterine pregnancy. The ovaries were not sonographically visible. A pelvic MRI was subsequently performed, which demonstrated a cystic mass measuring 3.1 x 2.8 x 3.4 cm contiguous with the right ovary, with a peripheral soft tissue nodule that measured 1.5 x 1.3 x 1.7 cm (Figure 1). The soft tissue nodule was predominantly lipid with an appearance that was characteristic of a right ovarian mature teratoma. NMDA receptor antibodies from the outside hospital and our institution returned as positive. On hospital day #3, the patient underwent an urgent laparoscopic right salpingo-oophorectomy. Examination of the right ovary by surgical pathology revealed a unilocular cyst measuring 3.5 cm in diameter and containing a 1.5 cm nodular excrescence (Rokitansky nodule) with adherent hair and sebaceous material, grossly consistent with a teratoma. Routine hematoxylin and eosin (H&E)-stained histologic sections confirmed the diagnosis of a mature cystic teratoma (dermoid cyst) with foci of mature neuroglial tissue located within the grossly nodular solid component (Figure 2A-B). Neuroglial elements included occasional binucleate neurons without prominent degenerative features (Figure 2C-D). Focal lymphoid aggregates without germinal centers were present in association with epithelial structures but not neuroglia. No additional histopathologic abnormalities were identified in the right adnexa.
In addition to tumor removal, she was treated with methylprednisolone, IVIG, and plasma exchange. On hospital day #9, a tracheostomy was performed for respiratory support secondary to failed extubation trials, and percutaneous endoscopic gastrostomy (PEG) tube was placed to meet ongoing nutritional demands. During the following 25 days after surgery, while in the neurological intensive care unit (ICU), the patient’s seizures ceased, and AEDs were down titrated. However, her clinical course was further complicated by agitation, sleep disturbance, and dysautonomia. On POD#2, while on prophylaxis consisting of Lovenox 40 mg daily, she was found to have a provoked non-occlusive left common femoral deep vein thrombosis (DVT) and was maintained on therapeutic low molecular weight heparin injections for the reminder of her pregnancy. The patient was subsequently discharged back to the original hospital facility on hospital day #25 for ongoing care, as it was geographically closer to the patient’s family for visitation. However, after 18 days at the outside hospital, the patient was transferred back to our institution at 20w5d for a higher level of care given concern for a possible hepatic abscess, as well as ongoing management of worsening agitation. At the outside hospital, the patient was noted to have rising liver function tests (AST 229 U/L, ALT 664 U/L, ALP 140 U/L), and a right upper quadrant ultrasound showed concern for a hepatic abscess. The patient was also noted to have increased agitation requiring scheduled haloperidol, olanzapine, quetiapine, and benzodiazepines. She continued to be non-verbal on exam with tracheostomy collar and PEG tube in place, receiving tube feeding for nutritional goals.
Maternal-fetal medicine was consulted to evaluate for obstetric causes of transaminitis, including preeclampsia, HELLP Syndrome, acute fatty liver of pregnancy, and intrahepatic cholestasis of pregnancy. A complete work-up was performed: the patient had normal blood pressures, otherwise reassuring preeclampsia labs, normal glucose and ammonia levels, and normal bile acids. It was discussed with the patient’s primary team that these diagnoses are exceedingly rare and unlikely at 20 weeks gestational age, and given the otherwise normal work-up, an obstetric cause of transaminitis was effectively ruled out. Hepatology was also consulted, with an unrevealing work-up. Given her ongoing transaminitis of unclear etiology, the Interventional Radiology team performed a liver biopsy on hospital re-admission day #9, with pathology most consistent with drug-induced liver injury. It was suspected the likely culprits included the prior phenytoin, fosphenytoin, and valproate, and current haloperidol, olanzapine, quetiapine, and benzodiazepines, all of which are metabolized by the liver. Her medications were optimized with the assistance of the neurology and psychiatry services, and her liver enzymes down-trended and normalized over the remainder of her pregnancy. The patient was followed by the maternal-fetal medicine team throughout the 108-day re-admission. After 24 weeks gestation, she was followed by twice weekly non-stress testing as well as monthly assessments of fetal growth, which all proved unremarkable. Her neurologic and psychiatric status slowly improved over time. She became awake, alert and oriented to place, was attentive, and appropriately responsive to questions with fluent speech. Her seizures remained in remission, and she was ultimately weaned to levetiracetam 500mg twice daily. She was able to sleep throughout the night, and she was weaned off all prior psychiatric medications and was maintained on ramelteon alone. She was able to increase her oral intake and she recovered motor function. She continued to have ongoing issues with recrudescence of NMDAR encephalitis as evidenced by ongoing difficulty with short-term and working memory, odd behaviors similar to her initial presentation (e.g. childlike smiles/laughter, shaking episodes), and occasional episodes of agitation (e.g. kicking staff, pulling at tracheotomy tube/peripheral IV).
On re-admission day #108 at 36w1d gestational age, the patient was transferred from the internal medicine unit at our adult hospital to the antepartum unit at our adjacent obstetric and children’s hospital. Her transfer of care involved several multidisciplinary team discussions between internal medicine, maternal-fetal medicine, obstetric anesthesia, and nursing. Antepartum nurses participated in additional training for tracheostomy and PEG tube care prior to the transfer. Speech-language-pathology (SPL), physical therapy (PT), occupational therapy (OT), nutrition, and respiratory therapy (RT) continued to be involved in her care upon transfer. Adult otorhinolaryngology (ENT) service followed the patient, and after discussion with the OB anesthesiology team, the tracheostomy was upsized from 4-0 to 6-0 on hospital day #7 in the event general anesthesia was going to be used during her case. During delivery planning, questions arose regarding the consent process for routine obstetrics care in the setting of profound short-term memory deficits and waxing and waning mental status. The hospital’s ethics team was consulted. The obstetrics team assessed that the patient had the capacity to assign her medical decision makers, and the patient was clear on multiple occasions that she opted for the father of the baby as well as her mother to make all medical decisions for her.
As the patient approached term, the fetus remained in breech presentation. Given that the patient had two prior vaginal deliveries, the patient and decision makers were counseled on external cephalic version (ECV), and the patient and the father of the baby provided consent for ECV, cesarean delivery, and post placental levonorgestrel intrauterine device (LNG-IUD) placement. On antepartum admission day #8 at 37w2d gestational age, the patient underwent an attempted ECV. During the procedure, the fetal heart rate (FHR) was noted to have prolonged bradycardia on ultrasound. The decision was made to proceed with an emergent cesarean delivery. A viable male infant was delivered in the breech position with APGARS 8,9 at 1,5 minutes weighing 3010 grams with blood tinged fluid on amniotomy. The surgery was uncomplicated with an estimated blood loss of 800 mL and a post-placental LNG-IUD was placed during the surgery. Her postpartum course was uncomplicated. On postpartum day #3, ENT decannulated her tracheostomy. Her newborn son was followed by well-baby nursery for routine newborn care without complications. On postpartum day #6, she was discharged with her newborn to her home with plans for close interval follow up with obstetrics, neurology, PT/OT, nutrition, and ENT services, as well as home health nursing and wound care services. At the time of hospital discharge, she would forget that she had delivered her baby until her memory was prompted regarding the delivery. She was eventually discontinued on levetiracetam, and 6 months post discharge, she continues to gradually recover. However, her short term memory continues to be affected.
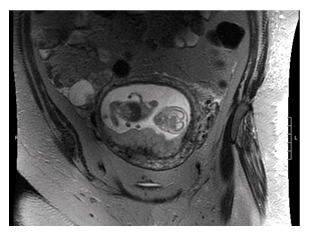
Figure 1: MRI of the pelvis without contrast. Gravid uterus with 3.4 cm mature teratoma visualized in the right ovary.
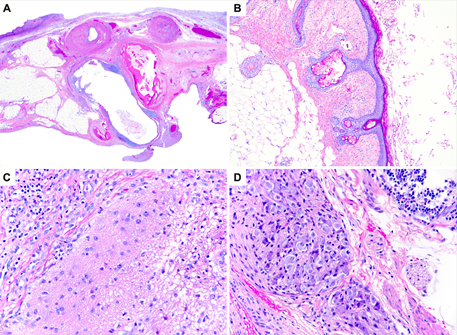
Figure 2: Mature cystic teratoma, hematoxylin and eosin-stained sections. A: Low-magnification view of solid component consisting of mature adipose tissue, bone, smooth muscle, neuroglia, and glandular epithelium surrounded by lymphoid aggregates (20x). B: Inner cyst wall lined by keratinizing squamous epithelium with associated sebaceous glands, underlying adipose tissue, and har follicle (100x). C-D: Mature neuroglial tissues with scattered infiltrating lymphocytes and plasma cells (400x).
3. Discussion
This case represents a severe form of anti-NMDA receptor encephalitis necessitating inpatient hospital care for the entirety of the patient’s pregnancy. Her hospital course illustrates the delicate balance of respecting and following the patient’s preferences while appreciating her limited working memory and the need to involve other caretakers in her ultimate decision making. Throughout her pregnancy, even during the previable period, this patient expressed a strong desire to continue her pregnancy. Due to the complex nature of her situation, it was deemed that the most optimal place for her to continue receiving care would be in a hospital setting. The patient was cared for by the intensive care, internal medicine, neurology, psychiatry, maternal-fetal medicine, obstetrics anesthesia, and otorhinolaryngology teams in a multidisciplinary fashion. She was also aided by the support of our speech-language pathologists, PT/OT, nutrition, and respiratory therapists. We utilized our ethics committee in assisting decision making capacity and in navigating surrogate decision makers for the patient. Creating this global care model ensured that the patient’s care and delivery timing was truly optimized.
In patients with anti-NMDA receptor encephalitis with an ovarian mass, approximately 80% of patients will have improvement in symptoms after its removal [5]. However, in pregnant patients, ovaries are often difficult to visualize due to the enlarging gravid uterus. While ultrasound is the preferred imaging both in pregnancy and in pelvic imaging, multiple case studies, including ours, did not visualize ovaries on pelvic ultrasound [6, 7]. Therefore, if a pregnant patient is presenting with symptoms of seizures, psychosis, and autonomic dysfunction with a high suspicion for anti-NMDAR encephalitis, if the ovaries are not visualized on ultrasound, additional imaging with pelvic MRI or CT should be performed to assist in making the diagnosis. Limited histopathologic studies of ovarian teratomas in patients with anti-NMDA receptor encephalitis has revealed that distinctive histologic features discriminate encephalitis-associated tumors from control teratomas in patients without neurologic symptoms. Specifically, the presence of prominent abnormal dysplastic or degenerative neurons and the co-localization of neuroglial tissue and reactive lymphoid aggregates with germinal centers are hallmark features of encephalitis-associated teratomas [8-10]. These microscopic clues to the clinical diagnosis were notably absent in the present case despite adequate tissue sampling. Although there is a need for further clinicopathologic study, it should be recognized that histopathologic examination of resected tumors has a limited, and generally late-stage, role in the diagnosis of anti-NMDA receptor encephalitis. This case underscores the importance of prompt recognition of the clinical characteristics of anti-NMDA receptor encephalitis and its expedient workup including adequate imaging studies and rapid CSF autoantibody testing to confirm the diagnosis and initiate early treatment.
In addition, women suffering from anti-NMDAR encephalitis after 20 weeks of gestation are often being evaluated for pre-eclampsia or eclampsia due to seizure activity [11, 12]. In our case, the patient had severely elevated liver function tests along with seizure activity at an outside hospital when she was transferred. Many antiepileptics and psychotropic medications may be hepatotoxic, and care should be taken in ruling out drug induced hepatotoxicity during workup so as not to perform a non-indicated iatrogenic preterm delivery. In addition, there was initial concern regarding the feasibility of performing an ECV with a PEG tube in place with the concern of dislodgement. However, given that there are few absolute contraindications to performing an ECV [13], we believed that it would be reasonable to attempt to perform this procedure, and while it was unsuccessful, still feel that this was a reasonable approach in attempting to offer this patient a vaginal delivery.
4. Conclusion
In conclusion, while anti-NMDAR encephalitis can be a debilitating disease in pregnancy, we found that a favorable outcome can be achieved through a strong multidisciplinary team guiding maternal care. And even with the constellation of this patient’s maternal complications, we were able to carry the pregnancy to term, with delivery of a healthy neonate and improved maternal neurological status.
Conflicts of Interest
Each named author has nothing to disclose and has substantially contributed to the care of the patient and this manuscript. The material presented is an original case report, has not been previously published or submitted for publication to any other journal. All authors have no conflict of interest to disclose. The patient, her partner, and the patient’s mother consented for this case to be written and published into a case report.
References
- Lynch DR, Rattelle A, Dong YN, et al. Anti-NMDA Receptor Encephalitis: Clinical Features and Basic Mechanisms. In: Advances in Pharmacology. Elsevier 82 (2018): 235-260.
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7 (2008): 1091-1098.
- Wang H. Efficacies of treatments for anti-NMDA receptor encephalitis. Front Biosci Landmark Ed 21 (2016): 651-663.
- Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12 (2013): 157-165.
- Dalmau J, Lancaster E, Martinez-Hernandez E, et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 10 (2011): 63-74.
- Chan LW, Nilsson C, Schepel J, et al. A rare case of anti-N-methyl-D-aspartate receptor encephalitis during pregnancy. N Z Med J 128 (2015): 3.
- Kim J, Park SH, Jung YR, et al. Anti-NMDA Receptor Encephalitis in a Pregnant Woman. J Epilepsy Res 5 (2015): 29-32.
- Nolan A, Buza N, Margeta M, et al. Ovarian Teratomas in Women With Anti-N-methyl-D-Aspartate Receptor Encephalitis: Topography and Composition of Immune Cell and Neuroglial Populations Is Compatible With an Autoimmune Mechanism of Disease. Am J Surg Pathol 43 (2019): 949-964.
- Dabner M, McCluggage WG, Bundell C, et al. Ovarian teratoma associated with anti-N-methyl D-aspartate receptor encephalitis: a report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol Off J Int Soc Gynecol Pathol 31 (2012): 429-437.
- Day GS, Laiq S, Tang-Wai DF, et al. Abnormal neurons in teratomas in NMDAR encephalitis. JAMA Neurol 71 (2014): 717-724.
- Xiao X, Gui S, Bai P, et al. Anti-NMDA-receptor encephalitis during pregnancy: A case report and literature review: Case report on anti-NMDA-R encephalitis. J Obstet Gynaecol Res 43 (2017): 768-774.
- Shahani L. Steroid unresponsive anti-NMDA receptor encephalitis during pregnancy successfully treated with plasmapheresis. Case Rep 2015 (2015).
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. External Cephalic Version: ACOG Practice Bulletin, Number 221. Obstet Gynecol 135 (2020): e203-e212.
Appendix
Appendix I: CSF laboratory studies
Stanford studies:
- CSF with lymphocytic pleocytosis (WBC 49 µL and 24 µL in tubes 1 and 4, respectively) normal protein/glucose. Elevated opening presusure at 33 cm H2O.
- CSF studies completed: Biofire - negative, HSV 1 and 2 PCRs - negative, VZV PCR - negative | Cytology - negative for malignant cells, HHV6 negative
- OGB 12/22 positive
- Serum autoimmune antibody panel: NMDA Ab positive
CSF studies from OSH 12/17:
Culture negative
Acid Fast Bacilli Smear negative
CSF Cryptococcus Ab - negative
HSV I & II DNA PCR - negative
Coccidioides source, Ab CF Curr, AB CF Prev, IgG, IgM - pending
Anti-NMDA Rec Ab (IFA) - positive, 1:256
Paraneoplastic panel, serum (PAVAL, Mayo Clinic) - negative
Appendix II: Relevant serum studies
Serum studies from OSH 12/17:
HCG, Quant 40,459
Blood cultures 12/16: negative
Utox 12/16: negative
HIV 1&2 Ag/Ab, 4th gen 12/16: 0.13
Urine, strep pneumoniae 12/17: final negative
Influenza A&B 12/17: negative
ANA screen - Negative
ANCA screen - Negative
c-ANCA titer - Negative
Atypical p-ANCA titer - Negative
Double Strand DNA Ab - Negative
Lyme IgG - Negative
Lyme IgM - Negative
St. Louis Encephal IgG - Negative
St. Louis Encephal IgM - Negative
West Equine Enceph IgG - Negative
West Equine Enceph IgM - Negative
QuantiFERON negative
RPR - Negative
Cocci IgM and IgG NONREACTIVE
EBV VCA Igi 34.4 (< 18)
Appendix III: EEG readings
EEG 1/3-4: diffuse slowing
EEG 1/2-3: diffuse slowing
EEG 1/1: diffuse slowing, no seizures
EEG 12/26-12/28: mild-moderate diffuse slowing of the background rhythms (including some rhythmical slowing). No electrographic seizures have been captured since 00:25am on 12/23/2019.
EEG 12/24/19-12/25/2019: mild to moderate slowing; left more than right temporal slowing. There are no extreme delta brushes on this record.
EEG 12/23/19-12/24/2019: mild to moderate slowing, left more than right temporal slowing.
EEG 12/22/2019 - 12/23/2019 focal status epilepticus with frequent but discontinuous bitemporal electrographic seizures (left >> right temporal seizures). Individual scalp seizure patterns lasted less than a minute and at worst occurred every ~2-10 minutes, but improving with treatment. The last seizure was at 00:25am on 12/23/2019 in this segment; mild to moderate slowing; left more than right focal temporal slowing.
