A Randomised Comparative Interventional Prospective Study of Intubation by Macintosh Laryngoscope Versus McGrath Video Laryngoscope in Patients Undergoing Cardiac Surgery
Article Information
Indu Verma1*, Chandan Verma2, Sandeep Dhaked3, Ramnaresh Sharma3
1Professor, Department of Anesthesia, SMS Medical college, Jaipur, India
2Associate Professor, Department of Pharmacology, SMS Medical college, Jaipur, India
3Resident, Department of Anesthesiology, SMS Medical college, Jaipur, India
*Corresponding Author: Indu Verma, Professor, Department of Anesthesia, SMS Medical college, Jaipur, India
Received: 22 May 2020; Accepted: 24 June 2020; Published: 30 June 2020
Citation: Indu Verma, Chandan Verma, Sandeep Dhaked, Ramnaresh Sharma. A Randomised Comparative Interventional Prospective Study of Intubation by Macintosh Laryngoscope Versus Macgrath Video Laryngoscope in Patients Undergoing Cardiac Surgery. Anesthesia and Critical Care 2 (2020): 052-065
Share at FacebookAbstract
Background: Laryngoscopy and endotracheal intubation is an integral part of general anesthesia for cardiac surgery. Direct laryngoscopy and passage of endotracheal tube through the larynx is a noxious stimulus, which can provoke untoward response in the cardiovascular, respiratory and other physiological systems. Significant tachycardia and hypertension can occur with tracheal intubation under light anesthesia. In this study our aim was to evaluate hemodynamic changes during intubation by using Macintosh and McGrath video laryngoscope in patients undergoing cardiac surgeries.
Objective: Our aim was to evaluate hemodynamic changes during intubation by using, Macintosh and McGrath video laryngoscope in patients undergoing cardiac surgeries.
Material and method: A total of 60 patients were randomly allocated to two groups which were divided according to intubation with Macintosh (Group A, n=30) versus McGrath (Group B, n=30). Both groups were studied by using Edwards EV 1000 flowtrac monitor with hemodynamic variable eg. stroke volume (SV), stroke vol. variation (SVV), Systematic vascular resistance (SVR), Stroke vol. index (SVI), cardiac output (CO), cardiac index (CI), BP (blood pressure)&PR (pulse rate). Patient undergoing various cardiac surgeries were included with ASA grade III & IV. Patient’s having coagulation abnormalities, pre -existing haematological, metabolic, hepatic, respiratory, renal disease were excluded. Intubation with more than 2 attempts and difficult intubation were also excluded.
Result: In group A the mean intubation time was 17.17 ± 3.03 sec. and in group B mean intubation time was 21.13 ± 3.04 sec. Among two groups significant (P<0.05) difference was observed between them. In group B there was a decrease in SVV, SVI, MAP, CI, SBP at 15 minutes post intubation, which was sta
Keywords
Mc Grath; Macintosh; Hemodynamics; Cardiac Surgery
Mc Grath articles, Macintosh articles, Hemodynamics articles, Cardiac Surgery articles
Mc Grath articles Mc Grath Research articles Mc Grath review articles Mc Grath PubMed articles Mc Grath PubMed Central articles Mc Grath 2023 articles Mc Grath 2024 articles Mc Grath Scopus articles Mc Grath impact factor journals Mc Grath Scopus journals Mc Grath PubMed journals Mc Grath medical journals Mc Grath free journals Mc Grath best journals Mc Grath top journals Mc Grath free medical journals Mc Grath famous journals Mc Grath Google Scholar indexed journals Macintosh articles Macintosh Research articles Macintosh review articles Macintosh PubMed articles Macintosh PubMed Central articles Macintosh 2023 articles Macintosh 2024 articles Macintosh Scopus articles Macintosh impact factor journals Macintosh Scopus journals Macintosh PubMed journals Macintosh medical journals Macintosh free journals Macintosh best journals Macintosh top journals Macintosh free medical journals Macintosh famous journals Macintosh Google Scholar indexed journals Hemodynamics articles Hemodynamics Research articles Hemodynamics review articles Hemodynamics PubMed articles Hemodynamics PubMed Central articles Hemodynamics 2023 articles Hemodynamics 2024 articles Hemodynamics Scopus articles Hemodynamics impact factor journals Hemodynamics Scopus journals Hemodynamics PubMed journals Hemodynamics medical journals Hemodynamics free journals Hemodynamics best journals Hemodynamics top journals Hemodynamics free medical journals Hemodynamics famous journals Hemodynamics Google Scholar indexed journals Cardiac Surgery articles Cardiac Surgery Research articles Cardiac Surgery review articles Cardiac Surgery PubMed articles Cardiac Surgery PubMed Central articles Cardiac Surgery 2023 articles Cardiac Surgery 2024 articles Cardiac Surgery Scopus articles Cardiac Surgery impact factor journals Cardiac Surgery Scopus journals Cardiac Surgery PubMed journals Cardiac Surgery medical journals Cardiac Surgery free journals Cardiac Surgery best journals Cardiac Surgery top journals Cardiac Surgery free medical journals Cardiac Surgery famous journals Cardiac Surgery Google Scholar indexed journals stroke volume articles stroke volume Research articles stroke volume review articles stroke volume PubMed articles stroke volume PubMed Central articles stroke volume 2023 articles stroke volume 2024 articles stroke volume Scopus articles stroke volume impact factor journals stroke volume Scopus journals stroke volume PubMed journals stroke volume medical journals stroke volume free journals stroke volume best journals stroke volume top journals stroke volume free medical journals stroke volume famous journals stroke volume Google Scholar indexed journals stroke vol. variation articles stroke vol. variation Research articles stroke vol. variation review articles stroke vol. variation PubMed articles stroke vol. variation PubMed Central articles stroke vol. variation 2023 articles stroke vol. variation 2024 articles stroke vol. variation Scopus articles stroke vol. variation impact factor journals stroke vol. variation Scopus journals stroke vol. variation PubMed journals stroke vol. variation medical journals stroke vol. variation free journals stroke vol. variation best journals stroke vol. variation top journals stroke vol. variation free medical journals stroke vol. variation famous journals stroke vol. variation Google Scholar indexed journals Systemic vascular resistance index articles Systemic vascular resistance index Research articles Systemic vascular resistance index review articles Systemic vascular resistance index PubMed articles Systemic vascular resistance index PubMed Central articles Systemic vascular resistance index 2023 articles Systemic vascular resistance index 2024 articles Systemic vascular resistance index Scopus articles Systemic vascular resistance index impact factor journals Systemic vascular resistance index Scopus journals Systemic vascular resistance index PubMed journals Systemic vascular resistance index medical journals Systemic vascular resistance index free journals Systemic vascular resistance index best journals Systemic vascular resistance index top journals Systemic vascular resistance index free medical journals Systemic vascular resistance index famous journals Systemic vascular resistance index Google Scholar indexed journals Systemic vascular resistance articles Systemic vascular resistance Research articles Systemic vascular resistance review articles Systemic vascular resistance PubMed articles Systemic vascular resistance PubMed Central articles Systemic vascular resistance 2023 articles Systemic vascular resistance 2024 articles Systemic vascular resistance Scopus articles Systemic vascular resistance impact factor journals Systemic vascular resistance Scopus journals Systemic vascular resistance PubMed journals Systemic vascular resistance medical journals Systemic vascular resistance free journals Systemic vascular resistance best journals Systemic vascular resistance top journals Systemic vascular resistance free medical journals Systemic vascular resistance famous journals Systemic vascular resistance Google Scholar indexed journals percentage of glottis opening articles percentage of glottis opening Research articles percentage of glottis opening review articles percentage of glottis opening PubMed articles percentage of glottis opening PubMed Central articles percentage of glottis opening 2023 articles percentage of glottis opening 2024 articles percentage of glottis opening Scopus articles percentage of glottis opening impact factor journals percentage of glottis opening Scopus journals percentage of glottis opening PubMed journals percentage of glottis opening medical journals percentage of glottis opening free journals percentage of glottis opening best journals percentage of glottis opening top journals percentage of glottis opening free medical journals percentage of glottis opening famous journals percentage of glottis opening Google Scholar indexed journals
Article Details
1. Introduction
Hypertension and tachycardia occur during tracheal intubation and is affected by various factors like the opioid used, the device used for intubation and of course the patient characteristics. It can lead to serious complications in patients having cardiac disease like myocardial infarction or brain hemorrhage. The anesthetist plays a pivotal role in minimizing these effects during tracheal intubation. Tachycardia and hypertension were higher in patients who had difficult intubation [1, 2]. Laryngoscopy alone stimulates the pressor response and sympatho-adrenal responses as laryngoscopy with intubation. Stimulation of the supra-glottic region by tissue tension caused by laryngoscopy leads to the sympatho-adrenal response [3]. This hemodynamic response can be deleterious in patients undergoing various cardiac surgeries under general anesthesia as it can alter the balance between myocardial oxygen demand and supply which can lead to cardiac arrhythmias, myocardial infarction and cerebro-vascular accidents [4]. The conventional use of Macintosh laryngoscope requires alignment of the oral and pharyngeal axes in order to view the larynx. This maneuver induces the sympathetic response and causes hemodynamic instability when direct laryngoscopy is used [5]. This can be avoided by using a supra-glottic airway device [6], fibre-optic laryngoscope or a video laryngoscope [7]. Using a McGrath laryngoscope may reduce the incidence of hypertension after tracheal intubation compared to a Macintosh laryngoscope. The McGrath laryngoscope is a novel intubating device which has a small camera and light source at the tip of the blade. This video laryngoscope provides a clear image of the vocal cords on the display screen attached to the handle. We hypothesized that a lower incidence of hypertension and tachycardia will be observed with a McGrath laryngoscope compared to a Macintosh laryngoscope. The aim of this study was to observe the mean intubation time and the hemodynamic changes during intubation while using the two types of laryngoscopes.
2. Materials and Method
This hospital based prospective randomised comparative interventional study was done in 60 patients undergoing various adult cardiac surgeries like valvular replacement, coronary artery bypass grafting, congenital heart disease correction etc under general anesthesia with permission from the institutional ethical committee and review board. The CTRI trial number is CTRI/2019/12/022256. Written informed patient consent was obtained from all patients for performance of cardiac surgery under general anesthesia after complete explanation about the study protocol and procedure. The study duration was from December 2019 to March 2020. Patients aged 18- 60 years of either sex with Height ≥ 150 cm and weight between 45-75 Kg of ASA grade III, IV, undergoing various cardiac surgeries with a duration of surgery from 3 hrs to 6 hrs were included in the study. The exclusion criteria included, patient’s not willing to give consent, any bleeding or coagulation abnormalities, any major pre-existing neurological, metabolic, hepatic, respiratory or renal disease, history of allergy or hypersensitivity to any anaesthetic drugs, and any anticipated difficult intubation during pre-anaesthetic check or difficult intubation with greater than two attempts.
2.1 Sample size
Sample size was calculated, as 30 subjects for each of two groups which would be required at 95% confidence limit and 80% power to verify the expected minimum difference of 0.9 (±1.04) seconds in endotracheal tube intubation in both groups.
2.2 Randomization
Randomization was done on the basis of inclusion and exclusion criteria, all adult patients who would undergo various cardiac surgeries were included in the study. Total 60 such eligible patients were selected on the first cum first basis and were allocated to one of the group using sealed envelope based randomised allocation method. The study was conducted in the following two groups of patients (Macintosh & McGrath VL). Each group consisted of 30 patients (n=30 per group).
- Group A (Macintosh) - (n=30) Patients intubated with Macintosh Laryngoscope.
- Group B (McGrath) - (n=30) Patients intubated with McGrath Video Laryngoscope.
On arrival in the operation theatre fasting status, written informed consent and PAC were checked. All the routine monitors were attached and the preoperative baseline vitals i.e heart rate (HR), Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Mean arterial pressure (MAP), SpO2 & ECG were noted. Intravenous line was secured, and fluid Ringer Lactate started. IJV cannulation was done in right internal jugular vein and femoral arterial cannulation performed under local anesthesia. Patients were pre-medicated with injection midazolam 0.05 mg/kg, fentanyl 5 microgram /kg and inj. ondansetron 4mg iv. Data were collected 5 minutes after premedication (just prior to intubation). Patient’s were pre- oxygenated with 100 % oxygen for three minutes. Induction was done with inj. etomidate 0.3 mg/kg iv until there was a loss of eyelash reflex and lack of response to verbal commands, Inj. rocuronium bromide 0.9 mg/kg iv was given to facilitate laryngoscopy and intubation. Data were collected just before intubation and at 0, 2, 5, 10 and 15 minutes after intubation. Surgery was allowed to commence after 15 minutes of intubation & anesthesia was maintained with 100% Oxygen, 1% isoflurane, Midazolam, fentanyl and vecuronium. After end of surgery patients were shifted to ICU on positive pressure ventilation. We defined following parameters for study:
- Hypotension was defined as SBP< 25% of baseline value or 90 mm Hg, whichever was lower.
- Hypertension was defined as SBP > 25% of baseline value or 150mm Hg whichever was higher.
- Tachycardia was defined as HR > 25% of baseline value.
- Bradycardia was defined as HR < 60 beats/min.
- Rate Pressure Product (RPP=HR × SBP) is a good indicator of oxygen consumption. The difference between both the groups was calculated. It allows you to calculate the interval workload on hemodynamic response.
If these episodes occurred during study period (within 15 minutes of intubation) appropriate management and /or intervention was done and case was excluded from the study.
|
Hemodynamic Response |
RPP |
|
High |
>30000 |
|
High intermediate |
25000-29999 |
|
Intermediate |
20000-24999 |
|
Low intermediate |
15000-19999 |
|
Low |
10000-14999 |
- Materials and Methods
2.1 Statistical analysis
All the data were entered on Excel sheet M.S Office Excel-2010 and analysed statistically using SPSS Statistical software (version.20.0.0) and XL Stat. All the quantitative data were summarized in the form of Mean ± SD. The difference between mean values of the two groups was analysed using ANOVA one way test and within groups using paired T-test. All the qualitative data were summarized in the form of proportions. The differences between proportions were analysed using Chi–square test. The levels of significance and α - error were kept 95% and 5% respectively, for all statistical analysis. P values <0.05 were considered as Significant (S) and P value > 0.05 as statistically not Significant (NS).
3. Results
There was no significant difference between the two groups regarding age, sex, height, weight and type of surgeries (p >0.05) (Table 1). There was no statistical difference between the two groups as regards to Mallampati and Comark Lehane (P= 0.365) classification scales.
3.1 Mean intubation time
The mean intubation period in group A was 17.17 ± 3.03 sec. and in group B mean intubation time was 21.13 ± 3.04 sec as shown in Table 2. Among the two groups significant statistical difference was observed (p value<0.001). There was a decrease in the SV from baseline in both the groups on comparison between the intergroup there was more decrease in SV in group B as compared to group A shown in Figure 1. But this was not statistically significant (p>0.05). The Stroke volume variation (SVV) shown in Figure 2 was more or less same in the group B from the baseline as compared to group A which showed slight elevation.
3.2 Systemic vascular resistance (SVR)
There was no significant difference between the baseline values of mean Systemic Venous Resistance (SVR) in both the groups (P=0.762). The SVR was more increased in group B as compared to group A, but statistically not significant (p value > 0.05) as shown in Figure 3.
3.3 Systemic vascular resistance index (SVRI)
There was no significant difference between the baseline values of mean Systemic Venous Resistance Index (SVRI) in both the groups (P=0.671). A slight increase was observed in group B but without any statistical significance (p value>0.05) as shown in Figure 4.
3.4 Cardiac output
There was no significant difference between the baseline values of mean stroke volume variation in both the groups (P=0.404). (It was 6.01 ± 3.25 for group A and 6.85 ± 4.46 for group B). There was more decrease in cardiac output in group A as compared to group B, which was statistically not significant (p value=0.703) as shown in Figure 5.
3.5 Cardiac index
There was no significant difference between the baseline values of mean stroke volume variation in both the groups (P=0.711). At 15 minutes post intubation the cardiac index was more decreased in group B but without any statistical significance (p value=0.85)as shown in Figure 6.
3.6 Heart rate (bpm)
The baseline heart rate in Group A was 97.87 +- 24.66 bpm and in Group B it was 93.90+-21.51 bpm with a p value > 0.05. There was a slight increase in heart rate in Group B at 2, 5 and 10 minutes which was not statistically significant with a p value > 0.05. At 15 minutes Group B showed an increase heart rate but in Group A it showed a decrease in heart rate but with a p value >0.05 as shown in Table 3.
3.7 Mean arterial pressure(MAP) mm Hg
The MAP in Gp A was 95.93+-19 mmHg and 98.70 +- 15.6 S.D mm Hg with a p value =0.535. Gp A showed a decrease in MAP as compared to Gp B but statistically not significant p >0.05. Gp B showed no change in MAP from baseline but there was no statistical significance p value > 0.05 Table 3.
3.8 Rate pressure product (RPP)
Both the groups showed a slight increase in RPP 2 minutes after intubation. Both showed a decrease at 15 min post intubation. The decrease was more in the Group B but was not statistically significant p> 0.05 Table 3.
|
Number of patient (60) |
Group-A (Macintosh) 30 patients |
Group- B (McGrath) 30 patients |
P value |
|||
|
Mean |
S.D. |
Mean |
S.D. |
|||
|
Sex |
M/F |
13/17 |
20/10 |
0.119 (NS) |
||
|
Age (in yrs) |
42.87 |
12.49 |
42.47 |
14.81 |
0.910 (NS) |
|
|
Height (cms) |
160.73 |
7.26 |
161.13 |
5.76 |
0.813 (NS) |
|
|
Weight (kg) |
53.77 |
7.38 |
57.90 |
10.15 |
0.076 (NS) |
|
|
BMI |
20.87 |
2.60 |
20.98 |
3.27 |
0.889 (NS) |
|
|
MPG (I/II/III) |
27/3/0 |
28/1/1 |
0.365 (NS) |
|||
|
CLG (I/II/III) |
27/3/0 |
28/1/1 |
0.365 (NS) |
|||
Table 1: Demographic profile.
|
Variables |
Group A |
Group B |
||
|
Mean |
SD |
Mean |
SD |
|
|
Intubation Time (sec.) |
17.17 |
3.03 |
21.13 |
3.04 |
|
P value |
p<0.001 (S) |
|||
Table 2: Distribution of Mean Intubation Time (Mean ± SD) (seconds).
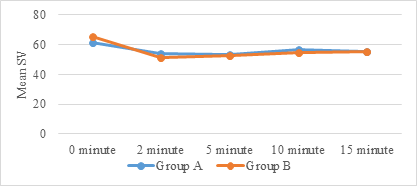
Figure 1: Distribution of Mean Stroke Volume (SV) (ml).
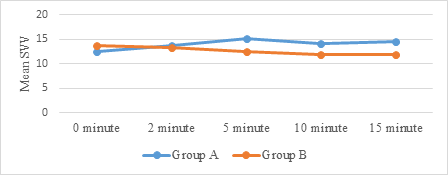
Figure 2: Distribution of Mean Stroke Volume Variation (SVV) (%).
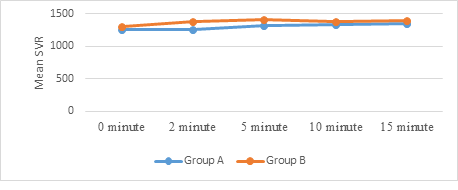
Figure 3: Distribution of Mean Systemic Venous Resistance (SVR) (dyne*second/cm5).
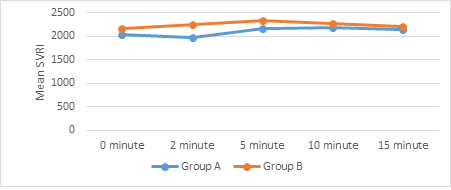
Figure 4: Distribution of Mean Systemic Venous Resistance Index (SVRI) (dyn*s/cm5*m2).
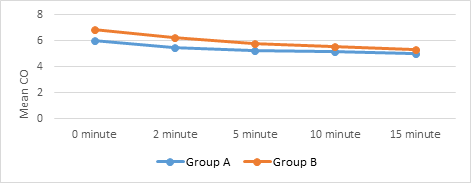
Figure 5: Distribution of Mean Cardiac Output (CO) (L/min.)
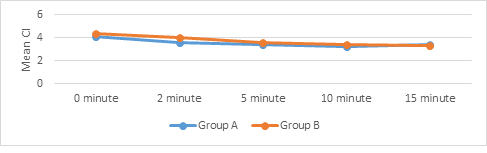
Figure 6: Distribution of Mean Cardiac Index (CI) (L/min./m2).
|
Group A |
Group B |
P value |
||||||
|
Mean |
SD |
Mean |
SD |
|||||
|
Mean Arterial Pressure (mmHg) |
||||||||
|
0 minute |
95.93 |
19.00 |
98.70 |
15.16 |
0.535 (NS) |
|||
|
2 minute |
90.50 |
18.37 |
98.47 |
17.33 |
0.089 (NS) |
|||
|
5 minute |
89.80 |
14.29 |
97.77 |
18.37 |
0.065 (NS) |
|||
|
10 minute |
91.93 |
16.91 |
92.30 |
12.75 |
0.924 (NS) |
|||
|
Pulse Rate (bpm) |
||||||||
|
0 minute |
97.87 |
24.66 |
93.90 |
21.51 |
0.509 (NS) |
|||
|
2 minute |
108.07 |
25.40 |
113.67 |
22.59 |
0.370 (NS) |
|||
|
5 minute |
102.47 |
23.61 |
103.60 |
21.54 |
0.846 (NS) |
|||
|
10 minute |
98.13 |
20.06 |
96.60 |
20.63 |
0.771 (NS) |
|||
|
15 minute |
93.87 |
20.91 |
95.03 |
20.28 |
0.827 (NS) |
|||
|
Rate Pressure Product |
||||||||
|
0 minute |
12413.77 |
4169.39 |
11873.87 |
3119.70 |
0.572 (NS) |
|||
|
2 minute |
13405.87 |
5337.18 |
14099.80 |
4118.91 |
0.575 (NS) |
|||
|
5 minute |
11718.43 |
3951.12 |
11987.27 |
3071.84 |
0.769 (NS) |
|||
|
10 minute |
11388.57 |
3319.45 |
10711.30 |
2613.82 |
0.383 (NS) |
|||
|
15 minute |
11007.13 |
3436.06 |
10429.37 |
2482.76 |
0.458 (NS) |
|||
Table 3: Hemodynamic parameters.
4. Discussion
The aim of our study was to evaluate the hemodynamic response to endotracheal intubation by using the conventional Macintosh laryngoscope and McGrath video laryngoscope in patients undergoing various adult elective cardiac surgeries. The primary objective of this study was to assess the time taken to intubate these patients. The secondary aim of this study was to investigate whether there was a significant difference in the hemodynamic parameters like H.R, MAP, SV, SVV, SVI, C.O, C.I, SVR and SVRI between both the groups. In the Present study we observed a better visualization of the larynx with McGrath VL as compared to Macintosh. Though the intubation time was prolonged in the VL. The intubation was easier in the McGrath VL but a good Laryngoscopic view does not always guarantee an easier intubation. The present study also found that- after using both Macintosh and McGrath VL for intubation in the patients undergoing cardiac surgery, hemodynamic variables were almost similar.
- The initial increase in the HR observed after intubation in both groups can be considered mild and clinically insignificant. There was no ST segment change during this period. The SBP also showed a decrease from the base line in both the groups but the DBP was more or less stable in group B. But was same after 15 min. Post intubation. Probably the anesthesia regime followed for intubation was accountable for this.
- The CO & CI were more or less the same in both the groups. But a slight decrease was seen in group A ,which was attributed to a decrease in SV and HR while it was less decreased in group B and the HR & SV were more in group B as compared to group A.
In our study Macintosh reduced the mean intubation time which was statistically significant. A recent study argued that video laryngoscope was superior to DL for the intubation in obstetric patients with normal airways [8]. Unlike a standard laryngoscope, the McGrath VL results in a glottis view without bringing into alignment the oral, laryngeal and pharyngeal axes. The McGrath VL results in a clear picture of the nearby airway anatomy and vocal cords on a display screen mounted on the handle [9]. Arici, et al. [8] showed that the McGrath VL provides a better glottis view associated with higher percentage of glottis opening (POGO) value and Comarck – Lehane grade. Several studies have shown that the glottis view is better with the McGrath VL than the Macintosh laryngoscope [10-13]. Shippey, et al. [14] showed that 88.9% of cases where a MG VL was used were of Cormack –Lehane grade I, while Jeon, et al. [15] reported a Cormacl-Lehane grade I of 96.3%, while the current study showed Cormack-Lehane gradeI and Mallampati grade I values of 93.33% in MG group. This suggests that MG VL is good in viewing the glottis opening as the blade angle of the MG VL is close to the axes of the tracheal aperture [16]. The initial increase in heart rate (HR) after intubation is mild and clinically significant. But the more increase in HR in McGrath group is because of the handling of the device probably more adaptability to the Macintosh. Tempe et al [17] showed a increase in HR also without any clinical significant. This is opposite to Colak F, et al. [18] who showed decreased in HR. There were no ST-T wave changes during this period. The SBP also showed a decrease from the baseline in both the groups but the diastolic BP (DBP) was more or less stable in group B. But was same after 15 minutes post intubation this is similar to study done by Colak F, et al. [18] probably the anesthesia regime followed for intubation was accountable for this. This is contrast to the study by Tempe, et al. [3] and similar to Sarkilar G, et al. [19]. Jeon, et al. [15] showed that there was a increase in systolic arterial blood pressure and heart rate while using the MGVL, while Arici et al. showed again an increase in the MAP and H.R during laryngoscopy with both the laryngoscopes. Weiss-Bloom, et al. [20] showed decreased hemodynamic responses to endotracheal intubation with induction by 5-10 microgram/kg Fentanyl and 0.3 mg/kg etomidate in patients scheduled for coronary artery bypass graft surgery.
The cardiac output and cardiac index decreased in both the groups and which was more in the McGrath group and was attributed to the decrease in SV. Although there was a mild rise in HR. Tempe, et al. [17] observed no change in cardiac output. These hemodynamic changes are suggestive of anesthetic effects taking over once the intubation response is stabilised. MAP was more or less stable in the McGrath group till 10 minutes post intubation while it decreased in the Macintosh group till 15 minutes post intubation which is in contrast to Tempe, et al. [17] while Colak F, et al. [18] showed a decrease in McGrath group. The SVRI was decreased at 2 minutes post intubation in group A and then increased at all levels in both the groups. This is similar to Tempe, et al. [17] though there was only mild elevation. Arici et al showed a higher mean intubation time in MG as compared to Macintosh. Mean intubation time of 47.25s for MG was observed in this study, while Taylor et al reported the mean intubation time of 35.8s with MG. Moreover, Shippey, et al. [14] showed a median time of 24.7s, whereas Walker, et al. [20] found that it was 47s with MG VL. Our study showed a mean intubation time of 21.7 seconds. This prolonged intubation time with McGrath video laryngoscope as compared to the Macintosh is attributed to various reasons. There was difficulty in navigating the ET tube to the glottis despite adequate visualization i.e. The eye hand co-ordination movement in most of the patients in McGrath group. The video laryngoscope blade occupies larger oral space than Macintosh blade. We observed that the tongue, which is not usually pushed to the left side while using video laryngoscope in contrast to Macintosh further decreased the space available to insert the ET tube into the oral cavity which required manuvering. Fogging of the McGrath VL lens due to expired gases inhibited clear visualisation of glottis was another reason for prolonging the duration of intubation. More experience with Macintosh may be another reason for quicker intubation as compared with McGrath video laryngoscope where the glottis inlet is intubated which requires hand eye co-ordination. Our study is similar to Toker MK, et al. [21] and Tempe, et al. [17]. Rate Pressure Product (RPP) is an index of myocardial oxygen consumption as shown by Globel FL, et al. [22]. A value exceeding 22000 may be associated with myocardial ischemia Robinson BF, et al. [23].
In our study in both groups the RPP which did not reach 15000 at any point of time, hence both the McGrath VL and Macintosh are safe to use in patients undergoing cardiac surgeries. Several studies have indicated that the glottic view is better with the McGrath VL than the Macintosh laryngoscope [8, 11, 14]. There was difficulty encountered while negotiating the endotracheal tube to the laryngeal opening in spite of having a good glottic visualization. In patients with McGrath VL this was the cause for prolongation of duration in this group . But in spite of this the hemodynamics were stable which is similar to Yokose M, et al. [24], they demonstrated that using a McGrath VL may reduce the incidence of hypertension after tracheal intubation compared to Macintosh laryngoscope, which is similar to our study. A Macintosh laryngoscope requires forcible alignment of the oropharyngeal axes to view the glottis whereas a video laryngoscope does not require even the shifting of tongue to left side which aids in a reduced hemodynamic response to intubation. Our study has some limitations. It was not possible to blind the intubating anaesthetist. All intubations were performed by experienced consultants, therefore the data may differ from others. The glottis view time was not recorded. Study population included only elective cardiac surgery with normal airway. The depth of anesthesia was not monitored, however the anaesthetic induction technique was similar in all patients.
References
- Rose DK, Cohen MM. The airway, problem and prediction in 18,500 patients. Can J Anaesth 41 (1994): 372-383.
- Elder JD, Dripps RD. Reflex circulatory response to direct laryngoscopy and tracheal intubation performed during general anesthesia. Anesthesiology 12 (1951): 556-566.
- Kamewad AK, SharmaVK, Popli V . Hemodynamic response to endotracheal intubation : direct versus video laryngoscopy. Int J Res Med sci 4 (2016): 5196-5250.
- Kanchi M, Nau HC, Banakal S, et al. Haemodynamic response to endotracheal intubation in coronary artery disease:Direct versus video laryngoscopy. Indian J Anaesth 55 (2011): 260-265.
- Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine response to laryngoscopy with and without tracheal intubation . Br.J Anaesth 59 (1987): 295-299.
- Akhlagh SH, Vaziri MT, MasoumiT, et al. Hemodynamic response to tracheal intubation via direct laryngoscopy and intubating laryngeal mask airway (ILMA) in patients undergoing coronary artery bypass graft (CABG). Middle East J Anaesthesiol 21 (2011): 99-103.
- Cooper RM, Pacey JA, Bishop MJ, et al. Early clinical experience with a new videolaryngoscope (GlideScope®) in 728 patients. Can J Anesth 52 (2005): 191-198.
- Arici S, Karaman S, Dogru S, et al. The McGrath series 5 video laryngoscope versus the Macintosh laryngoscope:A randomised trial in obstetric patients. Turkish J.Med Sci 44 (2014): 387-392.
- Nappens RR, Mobus S, Haid F, et al. Evaluation of the McGrath R series 5 video laryngoscopes after failed direct laryngoscopy. Anesthesia 65 (2010): 716-720.
- Ray DC, Billington C, Kearns PK, et al . A comparison of McGrath and Macintosh laryngoscopes in novice users: a manikin study. Anesthesia 64 (2009): 1207-1210.
- TaylorAM, PeckM, LauncelottS, et al . The McGrath-Series 5 videolaryngoscope vs the Macintosh laryngoscope: a randomised, controlled trial in patients with a simulated difficult airway. Anesthesis 68 (2013): 142-147.
- Wetsch WA, Carlitscheck M, Spelten O, et al. Success rates and endotracheal tube insertion times of experienced emergency physicians using five video laryngoscopes: a randomized trial in a simmulated trapped car accident victim. Eur J Anaesthesiol 28 (2011): 849-858.
- Dupanovic M, Isaacson SA, Borovacanin Z, et al. Messing SP Clinical comparison of two stylet angles for orotracheal intubation with the Glidescope video laryngoscope. J Clin Anesth 22 (2010): 352-359.
- Shippey B, Ray D, MckeownD. Case series:The McGrath video laryngoscope –an initial clinical evaluation. Can J Anesth 54 (2007): 307-313.
- Jeon WJ, Kim KH, Yeon JH, et al. A comparison of the Glidescope to the McGrath video laryngoscope in patients. Korean J Anesthiol 61 (2011): 19-23
- Shah PN, Das k. McGrath video laryngoscope may take a longer intubation time than Macintosh laryngoscope. J Anesthesiol (2015): 0-4.
- Deepak K Tempe , Kapil Chaudhary , Anitha Diwaker, et al . Comparison of hemodynamic response to laryngoscopy in patients undergoing coronary artery bypass grafting: A randomised prospective study. Annals of cardiac Anesthesia. Jan-Mar 9 (2016): 68-75.
- Colak F, Ozgul U, Erdogan MA, et al. Comparison of hemodynamic responses and QT c intervals to tracheal intubation with the McGrath MAC video laryngoscope and the Macintosh direct laryngoscope in elderly patients. Kaahsiung J Med Sci 35 (2019): 116-122.
- Sarikar G, Sargin M, Sartas TB, et al. Hemodynamic response to endotracheal intubation performed with video and direct laryngoscopy in patients scheduled for major cardiac surgery. Int J clin. expmed 8 (2015): 11477-11483.
- Walker L, Brampton W, Halai m, et al. Randomised controlled trial of intubation with the McGrath R series 5 video laryngoscope by inexperienced anaesthetists. Br J Anaesth 103/(3) (2009): 440-445.
- Toker MK, Altiparmak B, Karabay AG. Comparison of the McGrath video laryngoscope and macintosh direct laryngoscope in obstetric patients: A randomized controlled trial. Pak J Med Sci 35 (2019): 342-347.
- Globel FL, Nordstrom LA, Nelson RR, et al. The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 57 (1978): 549-556.
- Robinson BF. Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation 35 (1967): 1073-1083.
- Yokose M, Mihara T, Kuwahara S, et al. Effect of the McGrath video Laryngoscope on hemodynamic response during tracheal intubation: A Retrospective study. PLoSOne 11 (2016): e0155566.
